In continuation of my update on Tramadol
For older adults, initiation of tramadol is associated with an increased risk for hip fracture compared with initiation of codeine, ibuprofen, and other commonly used nonsteroidal anti-inflammatory drugs, according to a study published online Feb. 5 in the Journal of Bone and Mineral Research.
Jie Wei, Ph.D., from Central South University in Changsha, China, and colleagues examined the association between tramadol and the risk for hip fracture among individuals aged 50 years or older without a history of hip fracture, cancer, or opioid use disorder. Five sequential propensity score-matched cohort studies were assembled, including participants initiating tramadol (146,956 participants) or one of the following: codeine (146,956 participants), naproxen (115,109 participants), ibuprofen (107,438 participants), celecoxib (43,130 participants), or etoricoxib (27,689 participants).
The researchers identified 518 hip fractures in the tramadol cohort and 401 in the codeine cohort (3.7 versus 2.9/1,000 person-years) during one-year follow-up (hazard ratio, 1.28 for tramadol versus codeine). Hip fracture risk was higher in the tramadol cohort compared with the naproxen (2.9 versus 1.7/1,000 person-years; hazard ratio, 1.69), ibuprofen (3.4 versus 2.0/1,000 person-years; hazard ratio, 1.65), celecoxib (3.4 versus 1.8/1,000 person-years; hazard ratio, 1.85), and etoricoxib (2.9 versus 1.5/1,000 person-years; hazard ratio, 1.96) cohorts.
"Considering the significant impact of hip fracture on morbidity, mortality, and health care cost, our results point to the need to consider tramadol's associated risk of fracture in clinical practice and treatment guidelines," the authors write.
https://asbmr.onlinelibrary.wiley.com/doi/10.1002/jbmr.3933
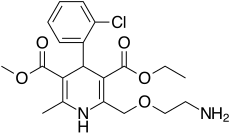
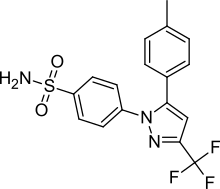
https://en.wikipedia.org/wiki/Tramadol
Tramadol Linked to Increased Hip Fracture Risk in Adults Aged ≥50