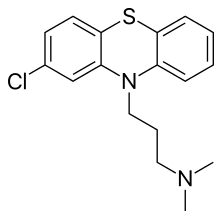
UT Southwestern Medical Center researchers find that an FDA-approved drug to treat high blood pressure seems to extend life span in worms via a cell signaling pathway that may mimic caloric restriction.
The drug, hydralazine, extended life span about 25 percent in two strains of C. elegans(roundworms), one a wild type and the other bred to generate high levels of a neurotoxic protein called tau that in humans is associated with Alzheimer's disease.
"This is the first report of hydralazine treatment activating the NRF2/SKN-1 signaling pathway. We found the drug extends the life span of worms as well as or better than other potential anti-aging compounds such as curcumin and metformin. The treatment also appeared to maintain their health as measured by tests of flexibility and wiggling speed," said Dr. Hamid Mirzaei, Assistant Professor of Biochemistry at UT Southwestern and senior author of the study, published today in Nature Communications.
The NRF2 pathway protects human cells from oxidative stress. The body's ability to protect itself against damaging oxygen free radicals diminishes with age, he said.
One of the hallmarks of aging and neurodegenerative diseases such as Alzheimer's and Parkinson's is oxidative stress, which is believed to result cumulatively from inflammatory and infectious illnesses throughout life, Dr. Mirzaei explained. SKN-1, a C. eleganstranscription factor, corresponds to NRF2 in humans. Both play a pivotal role in their respective species' responses to oxidative stress and life span, he said.
The UT Southwestern researchers were searching for a chemical probe they could use in experiments to identify proteins that get oxidized and become toxic during aging. Their screen for a substance that would cross the blood-brain barrier and be nontoxic led them to hydralazine.
"Age-related neurodegenerative diseases are devastating, and those conditions are on the rise due to the increase in the life span of humans. For that reason, it is important to develop treatments to maintain human health as long as possible," said Dr. Mirzaei, who is also an investigator in the Center for Alzheimer's and Neurodegenerative Diseases, part of the Peter O'Donnell Jr. Brain Institute at UT Southwestern.http://www.utsouthwestern.edu/newsroom/articles/year-2017/hbp-drug.html