The sodium-glucose cotransporter 2 inhibitor empagliflozin slows renal progression and averts clinical events, shows further analysis of the EMPA-REG OUTCOME trial.
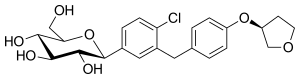 empagliflozin
empagliflozin
The previously reported primary analysis showed a reduced risk of major cardiovascular events in patients randomly assigned to take empagliflozin 10 or 25 mg daily, compared with placebo, in addition to their existing medication.
As now reported in The New England Journal of Medicine, the researchers found that microvascular events were also significantly less common in the 4132 patients taking either empagliflozin dose than in the 2068 taking placebo, at 14.0% versus 20.5%.
This was driven almost entirely by renal outcomes, report Christoph Wanner (Würzburg University Clinic, Germany) and team.
Incident or worsening nephropathy occurred in 12.7% of the empagliflozin group versus 18.8% of the placebo group, a significant 39% relative reduction. And 11.2% of patients taking empagliflozin versus 16.2% of those taking placebo progressed to macroalbuminuria, equating to a significant 38% risk reduction.
Patients in the empagliflozin group also had a significantly reduced risk of having a doubling of their serum creatinine level and requiring initiation of renal-replacement therapy.
During the first 4 weeks of treatment, patients taking empagliflozin had a reduction in their average estimated glomerular filtration rate (eGFR) of 0.62 and 0.82 mL/min per 1.73 m2 in the 10 and 25 mg dose groups, respectively. After this, however, eGFR in both groups remained relatively stable, with an annual decline of just 0.19 mL/min per 1.73 m2, compared with 1.67 mL/min per 1.73 m2 in the placebo group.
In an editorial that also refers to the just published LEADER trial, Julie Ingelfinger (Massachusetts General Hospital, Boston, USA) and Clifford Rosen (Maine Medical Center Research Institute, Scarborough, USA) agree with the LEADER investigators' view that differences in trial design and participant characteristics do not account for diabetes medications being cardioprotective in some studies but not others.
"We are left with differences that appear encouraging, yet are not a 'home run' with regard to the management of diabetes", they write.
The editorialists hope that, in the future, head-to-head trials of older and newer diabetes therapies "may help to delineate an even more effective treatment plan for the millions of people whose lives are affected by type 2 diabetes."
Ref : http://www.nejm.org/doi/full/10.1056/NEJMoa1515920#t=abstract
