In continuation of my update on tazarotene

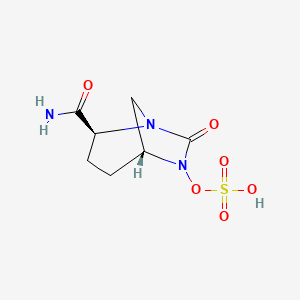
Ulobetasol 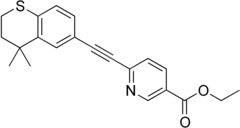
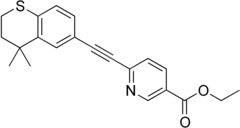
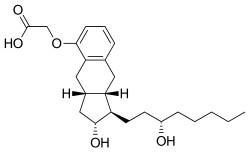
Tazarotene
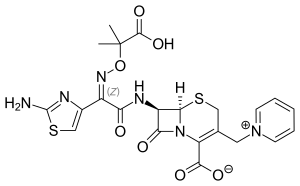
Bausch Health Companies Inc. (NYSE/TSX: BHC) and its dermatology business, Ortho Dermatologics, one of the largest prescription dermatology health care businesses, announced, that the U.S. Food and Drug Administration (FDA) has approved the New Drug Application for Duobrii (halobetasol propionate and tazarotene) Lotion, 0.01%/0.045%, indicated for the topical treatment of plaque psoriasis in adults. Duobrii is the first and only topical lotion that contains a unique combination of halobetasol propionate and tazarotene in one formulation. In a year-long safety study, patients used Duobrii Lotion for up to 24 weeks of continuous use and up to 52 weeks of as-needed use.2 Duobrii is expected to be available in June 2019.
"With today's approval of Duobrii, patients suffering from plaque psoriasis now have an innovative topical treatment option that uniquely combines two well-known ingredients, halobetasol propionate and tazarotene, with established safety profiles, into a single lotion featuring dual mechanisms of action," said Bill Humphries, president, Ortho Dermatologics. "Since psoriasis is a chronic skin disease, patients require continuous treatment in order to achieve optimal control of their symptoms. Now, with Duobrii, health care professionals and their patients have a new topical treatment option that can help them achieve those long-term goals. As a result, we believe that Duobrii has the potential to delay some patients from switching to more expensive biologic treatments, which could potentially result in health care savings."
Continued Mr. Humphries, "We remain committed to bringing forward new medicines, like Duobrii, to add to our portfolio of topicals and biologics to meet the varying treatment needs of patients with psoriasis."
When used separately to treat plaque psoriasis, the duration of use of halobetasol propionate is limited by FDA labeling constraints and the use of tazarotene can be limited due to tolerability concerns. By combining halobetasol propionate and tazarotene in an advanced, patented once-daily moisturizing lotion, the Duobrii formulation ensures uniform distribution, allowing for simultaneous contact with the skin surface.
In the United States, approximately 7.5 million people live with psoriasis, with 80 percent having plaque psoriasis.3 Plaque psoriasis is the most common type of psoriasis, a chronic, non-contagious skin disease that alters the life cycle of skin cells, causing them to build up rapidly on the surface of the skin.
"Duobrii provides the known benefits of a potent topical corticosteroid and a topical retinoid with synergistic efficacy. Combination therapy is the mainstay of topical treatment for plaque psoriasis, making Duobrii an important new option," said Linda Stein Gold, M.D., director, Dermatology Clinical Research, Henry Ford Health System. "Although effective, topical retinoids have had limited use as monotherapy due to tolerability concerns. Duobrii provides improved local tolerability, allowing patients to benefit from an extended duration of use."
https://en.wikipedia.org/wiki/Ulobetasol
https://en.wikipedia.org/wiki/Tazarotene