Knopp Biosciences LLC today announced the publication of a report in the journal Bloodthat a Phase 2 study of dexpramipexole in hypereosinophilic syndromes (HES) met its co-primary endpoints.
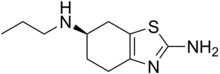
A team of investigators led by Dr. Amy Klion at the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), undertook the open-label study of dexpramipexole as a steroid-sparing agent in subjects with HES. Dexpramipexole had been observed to produce a significant, targeted reduction of peripheral blood eosinophils in earlier clinical trials in amyotrophic lateral sclerosis.
Subjects with HES on glucocorticoid therapy were eligible for the study if they required ≥10 mg prednisone or equivalent for control of symptoms and eosinophilia. Prior to study treatment, subjects underwent a standardized glucocorticoid taper to determine their minimally effective glucocorticoid dose (MED). Subjects for whom the MED had been determined within the past year or with an eosinophil count ≥1000/µL at the time of enrollment were eligible to proceed directly to dexpramipexole treatment at the discretion of the principal investigator. After 12 weeks of oral dexpramipexole treatment (150 mg twice daily) on a stable glucocorticoid dose, a glucocorticoid taper was attempted and the MED on dexpramipexole (MEDD) was determined.
The trial enrolled 10 subjects and met the co-primary endpoints of: 1) percentage of subjects experiencing a ≥50% reduction in MED and 2) reduction of glucocorticoid requirement among all subjects. Notably, three of the four responders meeting the primary endpoint exhibited complete hematological responses (eosinophil count of zero or near-zero) and were able to discontinue prednisone completely. These subjects have remained symptom-free, eosinophil-free, and steroid-free for 13-32 months while continuing dexpramipexole treatment, as reported in the article.
The investigators also reported that three of four responders who underwent biopsies had complete resolution of eosinophilia in affected skin or gastrointestinal tissue. Delayed and partial hematological responses were also noted in the trial.
Dexpramipexole was well tolerated, with no adverse events leading to drug interruption or discontinuation.
The article concluded, "Well-tolerated and with a dosing schedule convenient for routine outpatient treatment, dexpramipexole shows great promise as a novel oral therapy for HES."
Michael Bozik, M.D., President and CEO of Knopp Biosciences, said, "The Blood publication demonstrates that dexpramipexole merits Phase 3 development in HES, a rare hematological disease with significant morbidity and limited treatment options. We are grateful for our collaboration with Dr. Klion and her NIH colleagues, and we look forward to initiating the Phase 3 study later this year."
HES comprises a heterogeneous group of rare disorders characterized by peripheral eosinophilia and eosinophil-related end organ damage. The NIH trial enrolled subjects with the FIP1L1-PGDFRA-negative form of the disease, which accounts for 85-90% of all HES. Although glucocorticoid therapy is the first-line treatment for patients with FIP1L1-PGDFRA-negative HES, many patients develop serious side effects or resistance over time.
The Phase 2 study was conducted as part of an agreement between Knopp Biosciences and NIAID, demonstrating industry-government collaboration in the field of rare disease drug development.
Ref : http://knoppbio.com/news-events/show.php?40
Phase 2 study of dexpramipexole in hypereosinophilic syndromes meets its co-primary endpoints
