In continuation of my update on brivaracetam

UCB announced today that the U.S. Food and Drug Administration (FDA) has approved a supplemental new drug application (sNDA) for the company’s newest anti-epileptic drug (AED) Briviact (brivaracetam) oral formulations indicated as monotherapy and adjunctive therapy in the treatment of partial onset (focal) seizures in patients age four years and older.
This approval provides clinicians with the convenient option to prescribe Briviact to their pediatric patients as a tablet or oral solution, providing flexible administration options which are important considerations when treating children.
As the safety of Briviact injection has not been established in pediatric patients, Briviact injection is indicated for the treatment of partial-onset seizures only in patients 16 years of age and older.
As a result of the FDA’s decision, children age four years and older with partial-onset seizures in the U.S. can now be treated with Briviact. This extends the clinical application for Briviact which already has a similar indication for adults.
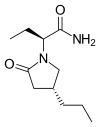
Briviact is the newest anti-epileptic drug (AED) in the synaptic vesicle protein 2A (SV2A) family of medicines – a class of medicines discovered and developed by UCB. Briviact demonstrates a high and selective affinity for SV2A in the brain. It is highly permeable and is rapidly and almost completely absorbed which may contribute to its anticonvulsant effects. Gradual dose escalation is not required when initiating treatment with Briviact for monotherapy or adjunctive therapy, allowing clinicians to initiate treatment at a therapeutic dose from day one.
“As a pediatric neurologist, one of the most challenging aspects in treating epilepsy in children is establishing, quickly, which anti-epilepsy drug will support them best in managing their seizures. The impact of poor seizure control can be extremely detrimental – both to overall quality of life for patients and caregivers and for a child’s development. There is a real sense of urgency for parents and healthcare providers to know whether a particular therapeutic approach is likely to be successful, minimizing some of the challenges associated with epilepsy and potentially allowing them to live a normal and active life,” explained Dr. James Wheless, Director, Neuroscience Institute & Le Bonheur Comprehensive Epilepsy Program - Le Bonheur Children’s Hospital. “The availability of an approved treatment option, such as Briviact, has potential to help improve the lives of children and their families by providing an additional choice to support them in their epilepsy journey.”
Epilepsy in childhood is a complex disorder that can have a significant impact on many aspects of a child's development and function. Pediatric epilepsy is the most common, serious neurological disorder among children and young adults, thought to affect nearly 470,000 children in the U.S.1,2 Social and societal stigma still associated with epilepsy can be especially cruel for children. The prevalence of pediatric epilepsy has been steadily increasing in the U.S.3 Today, it is estimated that nearly 470,000 children in the U.S. under the age of 18 have epilepsy, representing around a quarter of the total worldwide population who develop the condition each year.4 The U.S. Centers for Disease Control and Prevention (CDC) estimate that 0.6 percent of children in the U.S. ages 0 to 17 have active epilepsy – equivalent to six students in a school of 1000.5 Despite its growing prevalence, approximately 10 to 20 percent of pediatric epilepsy patients experience inadequate seizure control with available anti-epileptic drugs.6,7,8 Alongside close partnerships with educators, family members, and healthcare providers, there is a need for newer AEDs with better seizure control which can support and maximize a child’s potential for academic success.
“We believe there is a real need for newer AEDs to support and maximize the potential for success for children with epilepsy,” explained Jeff Wren, Executive Vice-President, Head of UCB’s Neurology Patient Value Unit. “The approval of Briviact in the U.S for pediatric patients represents an important milestone for patients, families, doctors, UCB, and the wider epilepsy community, and has the potential to provide additional value for patients - both today and for their future. We are very excited to be able to provide a new pediatric treatment choice, and we are proud to support patients as they progress on their epilepsy journey.”
The expanded FDA indication for Briviact is based on the principle of extrapolation of its efficacy data from adults to children, and is supported by safety and pharmacokinetics data collected in children. Adverse reactions in pediatric patients are generally similar to those seen in adult patients9. This principle of extrapolating clinical data from well controlled studies in adults has been recognized by the FDA as potentially addressing the challenge of limited pediatric data availability.
The safety and effectiveness of Briviact in the treatment of partial-onset seizures have been established in patients four years of age and older. Use of Briviact in these age groups is supported by evidence from placebo-controlled partial-onset seizure studies of Briviact in adults with additional pharmacokinetic and open-label safety studies in pediatric patients age 4 to younger than 16 years of age. Partial-onset seizures in pediatric patients aged 4 to 16 years of age are similar to those in adults and a similar AED exposure-response relationship has been demonstrated. Weight-based dose adaptations have been established in the pediatric population to achieve similar plasma concentrations as observed in adults. The safety and tolerability profile for Briviact in pediatric patients 4 to 16 years of age is generally similar to that seen with adult patients.
The most common adverse reactions recorded for adults (at least 5 percent for Briviact and at least 2 percent more frequently than placebo) are somnolence and sedation, dizziness, fatigue, and nausea and vomiting symptoms