Sun Pharmaceutical Industries Ltd, announced that Sun Pharma has received approval for Cequa (cyclosporine ophthalmic solution) 0.09%, from the U.S. Food and Drug Administration (FDA). Cequa is indicated to increase tear production in patients with keratoconjunctivitis sicca (dry eye).

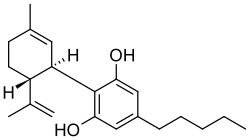
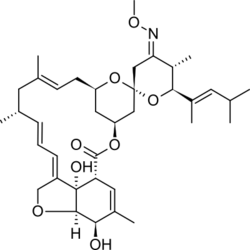
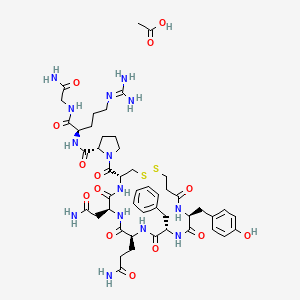
Cequa provides the highest FDA-approved concentration of cyclosporine A (CsA) and is the first and only approved CsA product that incorporates a nanomicellar technology. The innovative nanomicellar formulation allows the CsA molecule to overcome solubility challenges, penetrate the eye’s aqueous layer and prevents the release of the active lipophilic molecule prior to penetration. In the Phase 3 confirmatory trial on Cequa, after 12 weeks of treatment, as compared to vehicle, Cequa showed statistically significant improvement in the primary endpoint, Schirmer’s score (a measurement of tear production) (p<0.01). Improvements in secondary endpoints (i.e. ocular staining assessments) were seen as early as 1 month after initiating treatment. Cequa is dosed twice daily and will be available as a single-use vial.
The nanomicellar formulation technology uses micelles, which are gelatinous aggregates of amphipathic (both hydrophobic and hydrophilic) molecules formed at a well-defined concentration. The small size of the nanomicelles facilitates entry into corneal and conjunctival cells, enabling delivery of high concentrations of CsA.
“Dry Eye Disease represents an area of high unmet medical need, with a significant number of patients who are currently untreated,” said Abhay Gandhi, CEO, North America, Sun Pharma. “The U.S. FDA approval of Cequa represents a long-awaited dry eye treatment option and is an important milestone in the development of Sun’s Ophthalmics business. Cequa, with its novel nanomicellar formulation for a proven dry eye medication, delivers a lipophilic molecule in a clear solution form.”
Additionally, Jodi Luchs, MD, the principal investigator behind the Cequa confirmatory Phase 3 trial, noted: “Dry eye is a complex disease that lacks a ‘one-size-fits-all’ approach. As a clinician treating a high volume of dry eye patients, it’s important to have multiple treatment modalities available at my disposal. Given its strong clinical trial performance, the approval of Cequa is welcomed news, and I look forward to offering my patients this compelling new option.”
Cequa (cyclosporine ophthalmic solution) 0.09%, for topical ophthalmic use will be commercialized in the U.S. by Sun Ophthalmics, the branded ophthalmics division of Sun Pharma’s wholly owned subsidiary.
Sun Pharma Announces FDA Approval of Cequa (cyclosporine) Ophthalmic Solution to Treat Dry Eye Disease