In continuation of my update on Venetoclax
Patients whose acute myelogenous leukemia (AML) had relapsed or was resistant to chemotherapy and those who were deemed unable to tolerate chemotherapy experienced responses to the selective BCL-2 inhibitor venetoclax (Venclexta), with complete remissions in some, according to phase II clinical trial data.

Journal in Which the Study was Published: Cancer Discovery, a journal of the American Association for Cancer Research.
Authors: Senior author: Anthony Letai, MD, PhD, associate professor of medicine at Harvard Medical School and Dana-Farber Cancer Institute, in Boston, Massachusetts; Lead author: Marina Konopleva, MD, PhD, professor in the Department of Leukemia and the Department of Stem Cell Transplantation at The University of Texas MD Anderson Cancer Center in Houston
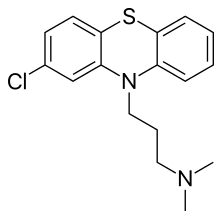
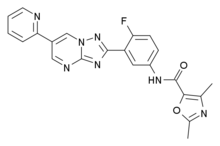
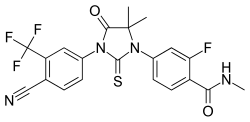
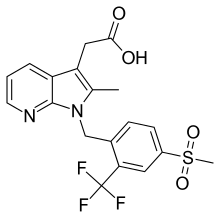
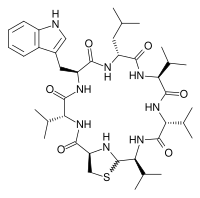
Background: Venetoclax is a small molecule that belongs to a class of drugs called BH3 mimetics. It binds with great affinity and selectivity to BCL-2, an antiapoptotic protein that plays a role in many blood cancers, Letai said. BCL-2 proteins keep the AML cells alive by binding to proapoptotic proteins. Venetoclax binds to BCL-2 and frees the proapoptotic proteins, thus rapidly and irreversibly forcing the AML cell to undergo apoptosis, he explained.
In April 2016, venetoclax was approved by the U.S. Food and Drug Administration for the treatment of certain patients with chronic lymphocytic leukemia (CLL).
How the Study Was Conducted: The study investigators recruited 32 patients with AML with a median age of 71 years to this multicenter, single-arm trial evaluating 800 mg daily oral venetoclax. Twenty-six patients received at least four weeks of therapy.
The investigators performed cytogenetic analysis, BH3 profiling, and next-generation sequencing to look for AML-related genetic mutations in the patients' samples collected at study entry and found that 12 patients had mutations in IDH genes, and six had a high BCL-2-sensitive protein index.
Results: The overall response rate was 19 percent; two patients had complete response (CR) and four had complete response with incomplete blood count recovery (CRi). The median duration of therapy in responders was 144.5 days, and the median duration of CR was 48 days. All patients discontinued therapy due to progressive disease or an adverse event, or for other reasons.
The four patients who had CRi had IDH mutations in their cancer cells. Response to the drug correlated with biomarker results, including indices of BCL-2 protein expression and BH3 profiling, Letai said. "This is significant as it supports the mechanism of action of venetoclax as an on-target inhibitor of BCL-2. Moreover, it offers the possibility of using BH3 profiling as a potential predictive biomarker for clinical use of BH3 mimetics," he added.