In continuation of my update on Afatinib
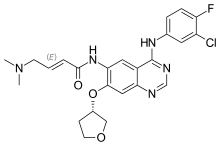
Patients with EGFR-activating mutations in advanced lung cancer seem to benefit more from afatinib than gefitinib as first-line treatment, researchers report at the first ESMO Asia 2015 Congress in Singapore.
In the global, randomised, open-label Phase IIb LUX-Lung 7 (LL7) trial1, the irreversible ErbB family blocker afatinib significantly improved efficacy versus gefitinib across a range of clinically relevant endpoints, such as progression-free survival, time-to-treatment failure and objective response rate. "Based on these results I would consider afatinib as the EGFR tyrosine kinase inhibitor (TKI) of choice for the first-line treatment for patients with EGFR mutation-positive non-small-cell lung cancer (NSCLC)," lead author, Professor Keunchil Park, head of the Division of Hematology/Oncology at Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, said.
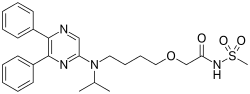
NSCLC is the most common type of lung cancer: activating epidermal growth factor receptor (EGFR) gene mutations are more frequently observed in non-smokers and women, and occur in 50% of Asians and only 10% of non-Asians. The targeted agents afatinib and gefitinib block key pathways involved in tumour growth and spread. They have both been approved for the treatment of naive patients, based on the results of Phase III trials, confirming their superiority compared to chemotherapy. Unlike the first-generation EGFR inhibitor gefitinib, the irreversible ErbB family blocker afatinib is suggested to be active in prolonging tumour response and delaying disease progression.