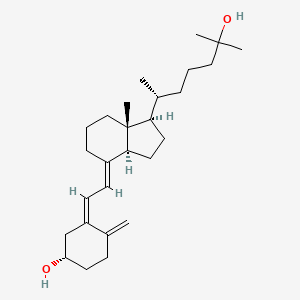
OPKO Health, Inc. announced that the U.S. Food and Drug Administration (FDA) has approved Rayaldee (calcifediol) extended release capsules for the treatment of secondary hyperparathyroidism (SHPT) in adults with stage 3 or 4 chronic kidney disease (CKD) and serum total 25-hydroxyvitamin D levels less than 30 ng/mL. Rayaldee is a patented extended release product containing 30 mcg of a prohormone called calcifediol (25-hydroxyvitamin D3).
"FDA's approval of Rayaldee represents an important milestone for OPKO," noted Dr. Phillip Frost, CEO and Chairman of OPKO. "Rayaldee is the first product to receive FDA approval for this important indication and is one of OPKO's many pharmaceutical products being developed for significant medical problems which will benefit from new treatment options."
Results from two 26 week placebo controlled, double blind phase 3 trials demonstrated that a larger proportion of stage 3 or 4 CKD patients with SHPT and vitamin D insufficiency achieved ≥30% reductions in plasma intact parathyroid hormone (iPTH) when treated with Rayaldee than with placebo. Vitamin D insufficiency was corrected in more than 80% of the patients receiving Rayaldee compared with less than 7% of subjects receiving placebo. Mean serum calcium and phosphorus levels increased by 0.1 mg/dL during Rayaldee treatment compared to placebo treatment, but these changes were deemed clinically irrelevant. No differences in Rayaldee's efficacy or safety were observed between patients with stage 3 CKD or stage 4 CKD.
"Rayaldee fills a large void in the current treatment options for SHPT in predialysis patients," commented Dr. Charles W. Bishop, CEO of OPKO's Renal Division. "The current standard of care is high dose vitamin D supplementation, an approach for treating SHPT that is neither FDA approved nor demonstrated to be safe and effective in this population. SHPT is a progressive disease that becomes increasingly debilitating and difficult to treat, necessitating timely and effective treatment."
"Rayaldee is an important new option for treating SHPT in patients with stage 3 or 4 CKD and vitamin D insufficiency," stated Kevin J. Martin, Director of Research, Division of Nephrology at Saint Louis University School of Medicine. "The great majority of SHPT cases in this patient population are associated with vitamin D insufficiency, a problem that Rayaldee can correct."
About Rayaldee
Rayaldee (calcifediol) extended release capsules are approved by the U.S. Food and Drug Administration (FDA) for the treatment of SHPT in adult patients with stage 3 or 4 CKD and serum total 25-hydroxyvitamin D levels less than 30 ng/mL. Rayaldee has a patented formulation designed to raise serum total 25-hydroxyvitamin D (prohormone) concentrations to targeted levels (at least 30 ng/mL) and to reduce elevated iPTH. OPKO expects to launch Rayaldee in the U.S. through its dedicated renal sales force in the second half of 2016. Rayaldee is not indicated in patients with stage 5 chronic kidney disease or end-stage renal disease on dialysis. The full prescribing information for Rayaldee will be available at www.opkorenal.com.
Potential side effects of Rayaldee include hypercalcemia (elevated serum calcium), which can also lead to digitalis toxicity, and adynamic bone disease with subsequent increased risk of fractures if intact PTH levels are suppressed by Rayaldee to abnormally low levels. Severe hypercalcemia may require emergency attention; symptoms of hypercalcemia may include feeling tired, difficulty thinking clearly, loss of appetite, nausea, vomiting, constipation, increased thirst, increased urination, and weight loss. Digitalis toxicity can be potentiated by hypercalcemia of any cause. Excessive administration of Rayaldee can cause hypercalciuria, hypercalcemia, hyperphosphatemia, or oversuppression of intact PTH. Common symptoms of vitamin D overdosage may include constipation, decreased appetite, dehydration, fatigue, irritability, muscle weakness, or vomiting. Patients concomitantly taking cytochrome P450 inhibitors, thiazides, cholestyramine, phenobarbital or other anticonvulsants may require dose adjustments and more frequent monitoring.
The most common adverse reactions in clinical trials (≥3% and more frequent than placebo) were anemia, nasopharyngitis, increased blood creatinine, dyspnea, cough, congestive heart failure and constipation.