In continuation of my update on amlodipine and celecoxib
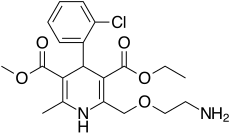
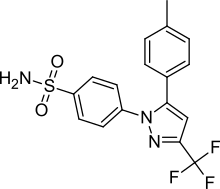
Kitov Pharma Ltd. an innovative bio pharmaceutical co., announced that the U.S. Food and Drug Administration (FDA) has approved Consensi (amlodipine and celecoxib) oral tablets for marketing. amlodipine celecoxib
Consensi is a patent-protected combination of celecoxib, a non-steroidal anti-inflammatory drug (NSAID), and amlodipine besylate, an antihypertensive calcium channel blocker. Consensi was approved for once daily use in three dosage forms, corresponding to the current approved dosages of amlodipine (2.5, 5, and 10 mg) for hypertension and a 200 mg dose of celecoxib for the treatment of osteoarthritis pain.
“We are very pleased with Consensi’s approval and would like to thank the members of Kitov’s team, consultants and investigators, as well as the FDA’s Division of Cardiovascular and Renal Products, for all of their support and assistance,” said Dr. J. Paul Waymack, Chairman of Kitov's Board and Chief Medical Officer. “Consensi provides a safe and effective combination treatment option for the millions of Americans who suffer from osteoarthritis pain and hypertension.
“Now that Consensi has been approved for marketing, our clinical and regulatory teams will focus on leveraging their drug development expertise to advance NT219, an exciting investigational new drug candidate currently in development for various oncology indications.”
Isaac Israel, Kitov’s CEO, added: “This approval demonstrates the Kitov team’s ability and experience in expertly guiding Consensi through clinical trials and regulatory review, from Investigational New Drug (IND) submission to FDA approval in less than four years.
“Over 50 million Americans suffer from osteoarthritis. About 1 of 3 U.S. adults or about 75 million people have high blood pressure*, known as the “silent killer” due to the absence of noticeable symptoms. As a result, patients’ adherence to the hypertension treatment regimen is low. We believe that Consensi, as a single pill combination treatment for osteoarthritis and hypertension, presents a unique value proposition of potentially increasing treatment adherence.
“We recently expanded our commercialization network for Consensi by securing a second licensing agreement in Asia with a major Chinese pharmaceutical company. The FDA approval of Consensi puts us in a stronger position towards securing commercial partnerships for the U.S. and other key territories.”
The FDA-approved Consensi New Drug Application included the positive results from the Company’s Phase III clinical trial. These data demonstrated that the study met its primary endpoint of showing that the drug lowers daytime systolic blood pressure by at least 50% of the reduction in blood pressure achieved in patients treated with amlodipine besylate only, with statistical significance of p=0.001. Kitov also submitted the positive results from its randomized double-blind, placebo-controlled renal function Phase III/IV clinical trial of Consensi. Data from this study validated the primary efficacy endpoint achieved in the completed Phase III clinical trial. This study also demonstrated that treatment with Consensi led to a statistically significant reduction of serum creatinine, a marker of renal function, from its baseline value (p=0.0005), demonstrating improved renal function in patients treated with the combination. In contrast, neither amlodipine besylate nor placebo lowered creatinine to a statistically significant level.



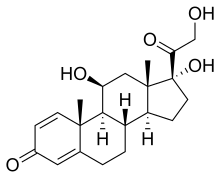 (Prednisole)
(Prednisole) (Indomethacin)
(Indomethacin)








