In continuation of my update on dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis) and edoxaban (Savaysa).
A new generation of blood thinners can reduce the risk of stroke in patients with atrial fibrillation, without requiring frequent monitoring and dietary restrictions.
But special attention must be given to the patient's age, kidney function and other factors before prescribing the new medications, according to a review article by neurologists at Loyola Medicine and Loyola University Chicago Stritch School of Medicine.
The report by Rochelle Sweis, DO and José Biller, MD, is published in the journal Current Treatment Options in Cardiovascular Medicine.
Atrial fibrillation (AFib) is the most common type of irregular heartbeat, and the prevalence is increasing as the population ages. In AFib, electrical signals that regulate the heartbeat become erratic. Instead of beating regularly, the upper chambers of the heart quiver and blood doesn't flow well. Blood clots can form, migrate to the brain and cause strokes. AFib is associated with a fivefold increase in the risk of stroke.
Blood thinning medications decrease the stroke risk by approximately 70 percent. For 60 years physicians have prescribed warfarin (Coumadin) and other blood thinners known as vitamin K antagonists. These medications have been proven to be effective in reducing the risk of blood clots and strokes. But they require continual monitoring and dose adjustments to ensure the drugs thin the blood enough to prevent clots, but not enough to increase the risk of major bleeding. Patients also must restrict their consumption of foods rich in vitamin K, such as spinach, Brussels sprouts, kale, parsley and green tea.
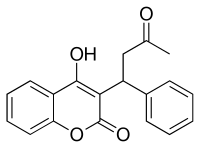
Warfarin
The new blood thinners include dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis) and edoxaban (Savaysa). In the right patient population, the new drugs are a safe and effective option for treating atrial fibrillation, Drs. Sweis and Biller write.
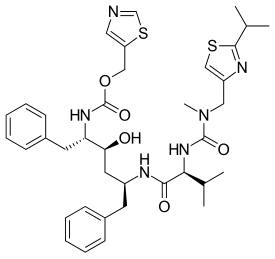
 Dabigatran
Dabigatran  Rivaroxaban (BAY 59-7939)
Rivaroxaban (BAY 59-7939)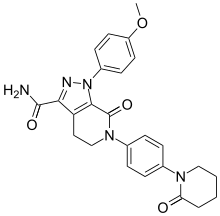 Apixaban
Apixaban  Edoxaban
Edoxaban
New oral blood thinners can decrease stroke risk in atrial fibrillation patients without frequent monitoring: A new generation of blood thinners can reduce the risk of stroke in patients with atrial fibrillation, without requiring frequent monitoring and dietary restrictions.