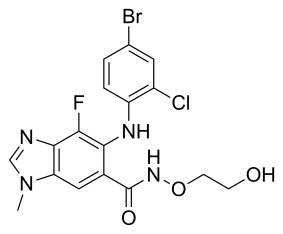
selumetinib
In an early-phase clinical trial of a new oral drug, selumetinib, children with the common genetic disorder neurofibromatosis type 1 (NF1) and plexiform neurofibromas, tumors of the peripheral nerves, tolerated selumetinib and, in most cases, responded to it with tumor shrinkage. NF1 affects 1 in 3,000 people. The study results appeared Dec. 29, 2016, in the New England Journal of Medicine.
The multicenter phase I clinical trial, which included 24 patients, was led by Brigitte C. Widemann, M.D., acting chief of the National Cancer Institute's (NCI) Pediatric Oncology Branch, and was sponsored by NCI's Cancer Therapy Evaluation Program. The study, conducted at the NIH Clinical Center and three participating sites, took advantage of techniques developed by Dr. Widemann's team that enabled very precise measurement of the plexiform neurofibromas. Experiments in mice that developed neurofibromas due to genetic modifications were performed at Cincinnati Children's Hospital in the laboratory of Nancy Ratner, Ph.D. NCI is part of the National Institutes of Health.
Plexiform neurofibromas develop in up to 50 percent of people with NF1. The majority of these tumors, which can cause significant pain, disability, and disfigurement, are diagnosed in early childhood and grow most rapidly prior to adolescence. Complete surgical removal of the tumors is rarely feasible, and incompletely resected tumors tend to grow back.
The primary aim of this clinical trial was to evaluate the toxicity and safety of selumetinib in patients with NF1 and inoperable plexiform neurofibromas, and, encouragingly, most of the selumetinib-related toxic effects were mild. At present, no therapies are considered effective for NF1-related large plexiform neurofibromas, but, in this trial, partial responses, meaning 20 percent or more reduction in tumor volume, were observed in over 70 percent of the patients.
Responses were observed in tumors that were previously growing at a rate of greater than 20 percent per year, as well as in non-progressing lesions. Tumor shrinkage was maintained long term, for approximately two years, and, as of early 2016, no disease progression had been observed in any trial participant. Additionally, anecdotal evidence of clinical improvement, such as a decrease in tumor-related pain, improvement in motor function, and decreased disfigurement, was reported.
"Some may say that a 20 percent volume reduction is too small to be meaningful, but to me, just stopping the growth of these devastating tumors is an important achievement," said Dr. Widemann. "The difference we see in these patients is truly unprecedented."
The disease-causing gene for NF1 was first identified in 1990 by two independent teams, one of them led by NIH Director Francis S. Collins, Ph.D., M.D., who at the time was chief of Medical Genetics at the University of Michigan. The other team was led by Ray White at the University of Utah. Research to understand the gene's function revealed that deregulation of the RAS signaling pathway was the most likely cause of tumor development. Numerous drugs that target RAS-related signaling pathways have been tested in patients with NF1 in phase I and phase II clinical trials, with disappointing results, hence the interest in selumetinib.
Selumetinib, provided for the study by AstraZeneca, is a selective inhibitor of the MEK protein, a part of the complex network of RAS signaling pathways. The drug has demonstrated activity in some advanced cancers, but it is not yet approved by the U.S. Food and Drug Administration for use in the United States. It is manufactured in capsule form to be taken orally.
Trial enrollment began in September 2011 and 24 children (11 girls, 13 boys) participated. Twice daily doses of the medicine were taken continuously, over a median of 30 month-long treatment cycles. The majority of patients are still continuing with therapy, some for as long as five years, and the long-term treatment has had no observed adverse effect on their development or overall health.
Experiments in mice with similar neurofibromas confirmed the inhibition of the MEK protein function in the tumors. Inhibition of the MEK protein diminished as early as two hours after drug administration. In addition, the animals received treatment with regular interruptions and still demonstrated tumor responses. This indicates that even limited MEK inhibition could cause tumor shrinkage in this disease.
"In the future, we may wish to look at intermittent dosing in patients to minimize toxicity and retain maximal outcomes," said Dr. Widemann.
In some patients, a loss of response to selumetinib with slow regrowth of tumors was observed, particularly after dose reductions. The researchers believe that additional studies are warranted to characterize tumors that no longer respond to selumetinib. NCI is currently sponsoring an ongoing phase II trial of the drug for adults with NF1, in which serial tissue samples are being obtained. This study should provide information about possible mechanisms of resistance to selumetinib.
In addition, a larger phase II pediatric trial is enrolling patients and should help establish the efficacy of selumetinib treatment in children. In this trial, in addition to tumor volume measurements, evaluations are being performed to assess the effect of selumetinib on plexiform neurofibroma related disfigurement, pain, quality of life, and function.
Ref : http://www.nejm.org/doi/full/10.1056/NEJMoa1605943
Read at : Med-News