Friday, March 19, 2021
Botanical drug is shown to help patients with head and neck cancers
Tuesday, March 9, 2021
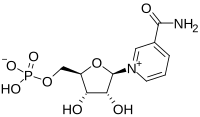
Discovery of compound that reverses the fertility clock

Newfound hope
Assisted reproductive technologies
Infertility by the numbers
Saturday, March 6, 2021
FDA Approves Ukoniq (umbralisib) for Marginal Zone Lymphoma and Follicular Lymphoma
Ukoniq is the first and only, oral, once daily, inhibitor of phosphoinositide 3 kinase (PI3K) delta and casein kinase 1 (CK1) epsilon. Accelerated approval was granted for these indications based on overall response rate (ORR) data from the Phase 2 UNITY-NHL Trial (NCT02793583). Continued approval for these indications may be contingent upon verification and description of clinical benefit in a confirmatory trial. This application was granted priority review for the MZL indication. In addition, Ukoniq was granted Breakthrough Therapy Designation (BTD) for the treatment of MZL and orphan drug designation (ODD) for the treatment of MZL and FL.
Michael S. Weiss, Executive Chairman and Chief Executive Officer of TG Therapeutics stated, “Today’s approval of Ukoniq marks a historic day for our Company with this being our first approval and we are extremely pleased to be able to bring our novel inhibitor of PI3K-delta and CK1-epsilon to patients with relapsed/refractory MZL and FL. We have built a commercial team with significant experience who will immediately start to engage our customers to educate them on Ukoniq and how to access the product for patients in need and expect to make Ukoniq available to US distributors in the next few days.” Mr. Weiss continued, “We want to thank the patients, physicians, nurses and clinical coordinators for their support and participation in our clinical trials, and the FDA for their collaboration throughout this process. We remain dedicated to patients with B-cell diseases and our mission of developing treatment options for those in need.”
“Despite treatment advances, MZL and FL remain incurable diseases with limited treatment options for patients who relapse after prior therapy and no defined standard of care. With the approval of umbralisib we now have a targeted, oral, once-daily option, offering a needed treatment alternative for patients,” stated Dr. Nathan Fowler, Professor of Medicine at The University of Texas MD Anderson Cancer Center and the Study Chair of the UNITY-NHL MZL &FL cohorts.
“The approval of umbralisib for the treatment of relapsed/refractory marginal zone lymphoma and follicular lymphoma offers patients a new treatment option, and new hope in the fight against these diseases,” stated Meghan Gutierrez, Chief Executive Officer of the Lymphoma Research Foundation.
The safety of Ukoniq monotherapy was based on a pooled population from the 221 adults with MZL and FL in three single arm, open label trials and one open label extension trial. Patients received Ukoniq 800 mg orally once daily. Serious adverse reactions occurred in 18% of patients who received Ukoniq. Serious adverse reactions that occurred in ≥2% of patients were diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%). The most common adverse reactions (>15%), including laboratory abnormalities, were increased creatinine (79%), diarrhea-colitis (58%, 2%), fatigue (41%), nausea (38%), neutropenia (33%), ALT increase (33%), AST increase (32%), musculoskeletal pain (27%), anemia (27%), thrombocytopenia (26%), upper respiratory tract infection (21%), vomiting (21%), abdominal pain (19%), decreased appetite (19%), and rash (18%).
Wednesday, March 3, 2021
Cabotegravir Injection Can Protect Women From HIV for Two Months
The drug cabotegravir is given every two months. It was 89 percent more effective at preventing HIV infection than Truvada pills, but both reduced the risk, the Associated Press reported. The study, which took place in Africa, was stopped early due to the promising results. The new findings echo those announced earlier this year from a study that compared the shots against the daily pills in gay men, the AP reported.
FDA Approves Tepmetko (tepotinib) as the First and Only Once-daily Oral MET Inhibitor for Patients with Metastatic NSCLC with METex14 Skipping Alterations
EMD Serono, the healthcare business sector of Merck KGaA, Darmstadt, Germany in the US and Canada, announced that the US Food and Drug Administration (FDA) has approved Tepmetko (tepotinib) following Priority Review for the treatment of adult patients with metastatic non-small cell lung cancer (NSCLC) harboring mesenchymal-epithelial transition (MET) exon 14 skipping alterations. This indication is approved under accelerated approval based on overall response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
The approval is based on results from the pivotal Phase II VISION study evaluating Tepmetko as monotherapy in patients with advanced NSCLC with METex14 skipping alterations.
"METex14 skipping occurs in approximately 3% to 4% of NSCLC cases, and patients with this aggressive lung cancer are often elderly and face a poor clinical prognosis," said Paul K. Paik, M.D., VISION primary investigator and Clinical Director, Thoracic Oncology Service, Memorial Sloan Kettering Cancer Center. "There is a pressing need for targeted treatments that have the potential to generate durable anti-tumor activity and improve the lives of patients with this challenging disease. Tepmetko offers an important and welcome new therapeutic option for patients with metastatic NSCLC harboring these genetic mutations."
"In recent years, the treatment of lung cancer has seen powerful progress in the understanding of the genetic mutations that lead to tumor growth, resistance and progression," said Andrea Ferris, President and CEO of LUNGevity. "The availability of a new precision medicine for NSCLC with METex14 skipping alterations advances patient access to targeted treatment and underscores the importance of routine comprehensive biomarker testing for patients with this challenging cancer."
Tepmetko is the first and only FDA approved MET inhibitor that offers once-daily oral dosing and is administered as two 225 mg tablets (450 mg). Patients with metastatic NSCLC should be selected for treatment with Tepmetko based on the presence of MET exon 14 skipping alterations.
"This approval of Tepmetko by the FDA is an important milestone on our mission to significantly improve the treatment of cancer where MET plays a driving role," said Danny Bar-Zohar, M.D., Global Head of Development for the Healthcare business of Merck KGaA, Darmstadt, Germany. "Our focus now is to ensure Tepmetko is accessible to patients in the United States and fully integrated into clinical practice given the important advance it represents for indicated patients as an oral once-a-day precision medicine."
EMD Serono, the healthcare business of Merck KGaA, Darmstadt, Germany in the US and Canada, is committed to providing patient access and reimbursement support for eligible Tepmetko patients through its Oncology Navigation Center™ (ONC) program in the US. ONC provides a spectrum of patient access and reimbursement support services intended to help US patients receive appropriate treatment access. ONC may be reached at 1-844-662-3631 (844-ONC-EMD1) between 8am-8pm Eastern Time, Monday through Friday, or by visiting OncNavigationCenter.com.
Tepmetko was the first oral MET inhibitor to receive a regulatory approval anywhere in the world for the treatment of advanced NSCLC harboring MET gene alterations, with its approval in Japan in March 2020. The FDA completed its review of Tepmetko under its Real-Time Oncology Review pilot program after previously granting the medicine Breakthrough Therapy Designation. The FDA also recently granted Tepmetko Orphan Drug Designation (ODD).
A Marketing Authorization Application for tepotinib for a similar indication was validated by the European Medicines Agency in November 2020. Applications have also been submitted in Australia, Switzerland, and Canada under the FDA's Project Orbis initiative, which provides a framework for concurrent submission and review of oncology medicines among international partners.1
In the study, Tepmetko demonstrated an overall response rate of 43% (95% CI, 32–56) in treatment-naïve patients (n=69) and 43% (95% CI, 33-55) in previously treated patients (n=83). Median duration of response (DOR) was 10.8 months (95% CI, 6.9-NE) and 11.1 months (95% CI, 9.5-18.5) among treatment-naïve and previously treated patients, respectively. Duration of response of six months or more occurred among 67% of treatment-naïve patients and 75% of previously treated patients, and duration of response of nine months or more occurred among 30% of treatment-naïve patients and 50% of previously treated patients.3
The safety population included 255 patients with NSCLC positive for METex14 skipping alterations, who received Tepmetko in the VISION study. Fatal adverse reactions occurred in one patient (0.4%) due to pneumonitis, one patient (0.4%) due to hepatic failure, and one patient (0.4%) due to dyspnea from fluid overload. Serious adverse reactions occurred in 45% of patients who received Tepmetko. Serious adverse reactions occurring in >2% of patients included pleural effusion (7%), pneumonia (5%), edema (3.9%), dyspnea (3.9%), general health deterioration (3.5%), pulmonary embolism (2%), and musculoskeletal pain (2%). The most common adverse reactions (≥20%) in patients who received Tepmetko were edema, fatigue, nausea, diarrhea, musculoskeletal pain, and dyspnea.
Tuesday, March 2, 2021
FDA Approves Cosela (trilaciclib) to Decrease the Incidence of Chemotherapy-Induced Myelosuppression
G1 Therapeutics, Inc. (Nasdaq: GTHX), a commercial-stage oncology company, announced the U.S. Food and Drug Administration (FDA) approval of Cosela (trilaciclib) for injection to decrease the incidence of chemotherapy-induced myelosuppression in adult patients when administered prior to a platinum/etoposide-containing regimen or topotecan-containing regimen for extensive-stage small cell lung cancer (ES-SCLC). It is the first and only therapy designed to help protect bone marrow (myeloprotection) when administered prior to treatment with chemotherapy. Cosela is expected to be commercially available through G1’s specialty distributor partner network in early March.
“The approval of trilaciclib (Cosela) is an important advance in the treatment of patients with extensive-stage small cell lung cancer receiving chemotherapy,” said Dr. Jeffrey Crawford, Geller Professor for Research in Cancer in the Department of Medicine and Duke Cancer Institute. “The most serious and life-threatening side effect of chemotherapy is myelosuppression, or damage to the bone marrow, resulting in reduced white blood cells, red blood cells and platelets. Chemotherapy-induced myelosuppression may lead to increased risks of infection, severe anemia, and/or bleeding. These complications impact patients’ quality of life and may also result in chemotherapy dose reductions and delays. To date, approaches have included the use of growth factor agents to accelerate blood cell recovery after the bone marrow injury has occurred, along with antibiotics and transfusions as needed. By contrast, trilaciclib provides the first proactive approach to myelosuppression through a unique mechanism of action that helps protect the bone marrow from damage by chemotherapy. In clinical trials, the addition of trilaciclib to extensive-stage small cell lung cancer chemotherapy treatment regimens reduced myelosuppression and improved clinical outcomes. The good news is that these benefits of trilaciclib will now be available for our patients in clinical practice.”
Chemotherapy is an effective and important weapon against cancer. However, chemotherapy does not differentiate between healthy cells and cancer cells. It kills both, including important hematopoietic stem and progenitor cells (HSPCs) in the bone marrow that produce white blood cells (immune cells that help fight infection), red blood cells (cells that carry oxygen from the lungs to the tissues), and platelets (cells that prevent bleeding from cancer, surgeries, chronic diseases, and injuries). This chemotherapy-induced bone marrow damage, known as myelosuppression, can lead to increased risk of infection, anemia, thrombocytopenia, and other complications. Myeloprotection is a novel approach of protecting HSPCs in the bone marrow from chemotherapy-induced damage. This approach can help reduce some chemotherapy-related toxicity, making chemotherapy safer and more tolerable, while also reducing the need for reactive rescue interventions.
“Chemotherapy is the most effective and widely used approach to treating people diagnosed with extensive-stage small cell lung cancer; however, standard of care chemotherapy regimens are highly myelosuppressive and can lead to costly hospitalizations and rescue interventions,” said Jack Bailey, Chief Executive Officer at G1 Therapeutics. “Cosela will help change the chemotherapy experience for people who are battling ES-SCLC. G1 is proud to deliver Cosela to patients and their families as the first and only therapy to help protect against chemotherapy-induced myelosuppression.”
Cosela is administered intravenously as a 30-minute infusion within four hours prior to the start of chemotherapy and is the first FDA-approved therapy that helps provide proactive, multilineage protection from chemotherapy-induced myelosuppression. The approval of Cosela is based on data from three randomized, placebo-controlled trials that showed patients receiving Cosela prior to the start of chemotherapy had clinically meaningful and statistically significant reduction in the duration and severity of neutropenia. Data also showed a positive impact on red blood cell transfusions and other myeloprotective measures. The trials evaluated Cosela in combination with carboplatin/etoposide (+/- the immunotherapy atezolizumab) and topotecan chemotherapy regimens. Approximately 90% of all patients with ES-SCLC will receive at least one of these regimens during the course of their treatment.
The majority of adverse reactions reported with Cosela were mild to moderate in severity. The most common adverse reactions (≥10%) were fatigue, hypocalcemia, hypokalemia, hypophosphatemia, aspartate aminotransferase increased, headache, and pneumonia. Serious adverse reactions occurred in 30% of patients receiving Cosela. Serious adverse reactions reported in >3% of patients who received Cosela included respiratory failure, hemorrhage, and thrombosis. Grade 3/4 hematological adverse reactions occurring in patients treated with Cosela and placebo included neutropenia (32% and 69%), febrile neutropenia (3% and 9%), anemia (16% and 34%), thrombocytopenia (18% and 33%), and leukopenia (4% and 17%), respectively.
“Quite often, people diagnosed with extensive-stage small cell lung cancer rely on chemotherapy to not only extend their lives, but also to acutely alleviate their symptoms,” said Bonnie J. Addario, lung cancer survivor, co-founder and board chair of the Go2 Foundation for Lung Cancer. “Unfortunately, the vast majority will experience chemotherapy-induced side effects, resulting in dose delays and reductions, and increased utilization of healthcare services. G1 shares our organization’s goal to improve the quality of life of those diagnosed with lung cancer and to transform survivorship among people living with this insidious disease. We are thrilled to see new advancements that can help improve the lives of those living with small cell lung cancer.”
Approximately 30,000 small cell lung cancer patients are treated in the United States annually. G1 is committed to helping patients with extensive-stage small cell lung cancer in the U.S. gain access to treatment with Cosela. For more information on access and affordability programs, patients and providers should call the G1toOne support center at 833-G1toONE (833-418-6663) from 8:00 a.m. to 8:00 p.m. Eastern time.
G1 received Breakthrough Therapy Designation from the FDA in 2019 based on positive data in small cell lung cancer patients from three randomized Phase 2 clinical trials. As is common with breakthrough-designated products that receive priority review, G1 will conduct certain post-marketing activities, including in vitro drug-drug interaction and metabolism studies, and a clinical trial to assess impact of trilaciclib on disease progression or survival in patients with ES-SCLC with chemotherapy-induced myelosuppression treated with a platinum/etoposide-containing or topotecan-containing regimen with at least a two year follow up. G1 intends to initiate the post-approval clinical trial in 2022.
Cosela (trilaciclib) Co-Promotion Agreement with Boehringer Ingelheim
In June 2020, G1 announced a three-year co-promotion agreement with Boehringer Ingelheim for Cosela in small cell lung cancer in the U.S. and Puerto Rico. G1 will lead marketing, market access and medical engagement initiatives for Cosela. The Boehringer Ingelheim oncology commercial team, well-established in lung cancer, will lead sales force engagement initiatives. G1 will book revenue and retain development and commercialization rights to Cosela and pay Boehringer Ingelheim a promotional fee based on net sales. The three-year agreement does not extend to additional indications that G1 is evaluating for trilaciclib. Press release details of the G1/ Boehringer Ingelheim agreement can be found here.
Monday, March 1, 2021
FDA Approves Amondys 45 (casimersen) Injection for the Treatment of Duchenne Muscular Dystrophy (DMD) in Patients Amenable to Skipping Exon 45
In continuation of my update on antisense oligonucleotides
Sarepta Therapeutics, Inc. the leader in precision genetic medicine for rare diseases, today announced that the U.S. Food and Drug Administration (FDA) has approved Amondys 45 (casimersen). Amondys 45 is an antisense oligonucleotide from Sarepta’s phosphorodiamidate morpholino oligomer (PMO) platform, indicated for the treatment of Duchenne muscular dystrophy (DMD) in patients with a confirmed mutation amenable to exon 45 skipping. This indication is based on a statistically significant increase in dystrophin production in skeletal muscle observed in patients treated with Amondys 45, which is reasonably likely to predict clinical benefit for those patients who are exon 45 amenable. Consistent with the accelerated approval pathway, the continued approval of Amondys 45 may be contingent on confirmation of a clinical benefit in confirmatory trials.
The ESSENCE trial – a placebo-controlled confirmatory trial to support the Amondys 45 approval – is ongoing and expected to conclude in 2024.
Although kidney toxicity was not observed in the clinical studies with Amondys 45, kidney toxicity, including potentially fatal glomerulonephritis, has been observed after administration of some antisense oligonucleotides. Kidney function should be monitored in patients taking Amondys 45. In the clinical trial, the most common adverse reactions observed in at least 20% of patients treated with Amondys 45 and at least 5% more frequently than in placebo were (Amondys 45, placebo): upper respiratory tract infections (65%, 55%), cough (33%, 26%), fever (33%, 23%), headache (32%, 19%), joint pain (21%, 10%), and pain in mouth and throat (21%, 7%).
“This is an important day for Sarepta and, far more importantly, for the patients that we serve. After years of scientific commitment, investment and development, the approval of Amondys 45, Sarepta’s third approved RNA therapy, offers treatment to the 8% of the DMD community who have a confirmed exon 45 amenable mutation,” said Doug Ingram, president and chief executive officer, Sarepta. “Along with our other approved RNA therapies, we can now offer treatment options for nearly 30% of Duchenne patients in the U.S. And our commitment to bring therapies to the greatest percentage of the DMD community as soon as possible continues.”
“Decades of research and commitment have fueled and now accelerate our progress towards new treatments for Duchenne,” said Marissa Penrod, founder of Team Joseph and parent of an 18-year old with Duchenne. “The extraordinary diligence and persistence of the Duchenne community – patients and families, clinicians and researchers – have led us to today’s approval, where we now have exon-skipping treatments for almost a third of those with Duchenne.”
Wednesday, February 10, 2021
FDA Approves Klisyri (tirbanibulin) for the Treatment of Actinic Keratosis on the Face or Scalp
Athenex, Inc., (NASDAQ: ATNX), a global biopharmaceutical company dedicated to the discovery, development, and commercialization of novel therapies for the treatment of cancer and related conditions, announced the U.S. Food and Drug Administration (FDA) approval of Klisyri (tirbanibulin) for the topical treatment of actinic keratosis (AK) on the face or scalp. Klisyri is the first FDA approved branded proprietary product for Athenex and will be launched in partnership with Almirall in the U.S. during the first quarter of 2021. Klisyri will be manufactured by Athenex, highlighting the vertically integrated capabilities of the company ranging from a preclinical lead to a developed product for market launch.
“The FDA approval of Klisyri is a significant milestone for Athenex. Klisyri is a home-grown product discovered and characterized by Athenex scientists and developed from pre-IND to NDA by the Athenex team. We are extremely proud of our team’s excellent execution,” said Dr. Johnson Lau, Chairman and Chief Executive Officer of Athenex. “Approval demonstrates our ability to execute upon the entirety of the drug development and registration process. We are excited to partner with Almirall to bring this first-in-class microtubule inhibitor to patients with actinic keratosis in the US.”
Dr. Rudolf Kwan, Chief Medical Officer of Athenex added, “The FDA approval of tirbanibulin ointment represents a first-in-class microtubule inhibitor for the treatment of actinic keratosis. We believe this small molecule platform has the potential beyond actinic keratosis and are leveraging the platform to develop therapies for other oncology indications.”
Mr. Peter Guenter, CEO of Almirall, stated, “We are delighted to partner with Athenex to market Klisyri in the U.S. and in Europe. This approval from the FDA represents a new option for Dermatologists and marks an important further step for Actinic Keratosis patients. What makes this new therapy particularly exciting is the 5-day course of treatment and its good tolerability. We look forward to the launch of Klisyri in the US in the first quarter of 2021.”
The FDA approved Klisyri based on the data from two pivotal, randomized, double-blind, vehicle-controlled Phase III studies (KX01-AK-003 and KX01-AK-004) that evaluated the efficacy and safety of Klisyri (tirbanibulin) ointment 1% in 702 adults with actinic keratosis of the face or scalp. Tirbanibulin demonstrated complete clearance of actinic keratosis lesions at day 57 in treated face or scalp areas in a significantly higher number of patients compared to vehicle. The most common adverse events were application site pruritus and pain reported by 9% and 10% of treated patients, respectively.
Actinic keratosis is a pre-cancerous skin lesion and is the second most common diagnosis made by dermatologists in the United States. If left untreated, 10-15% of AK lesions will develop into skin cancers.
Athenex has partnered with Almirall (Almirall, S.A., BME: ALM) to market Klisyri for the treatment of actinic keratosis on the face or scalp in the US and EU (including Russia) markets. In addition to the partnership with Almirall, Athenex has partnered with PharmaEssentia (6446.TWO) for actinic keratosis in Taiwan and has partnered with Xiangxue Pharmaceuticals (SHE:300147) for actinic keratosis in China, Hong Kong, and Macau.
https://en.wikipedia.org/wiki/Tirbanibulin
Tuesday, February 9, 2021
FDA Approves Orgovyx (relugolix) as the First Oral Gonadotropin-Releasing Hormone (GnRH) Receptor Antagonist for Advanced Prostate Cancer
Myovant Sciences (NYSE: MYOV), a healthcare company focused on redefining care for women and for men, today announced that the U.S. Food and Drug Administration (FDA) has approved Orgovyx (relugolix) for the treatment of adult patients with advanced prostate cancer. Orgovyx, which was granted Priority Review by the FDA, is the first and only oral gonadotropin-releasing hormone (GnRH) receptor antagonist for men with advanced prostate cancer. The approval is based on efficacy and safety data from the Phase 3 HERO study of Orgovyx in men with advanced prostate cancer. Orgovyx is expected to be available in January 2021.
“I am enormously pleased by the approval of Orgovyx and believe it has the potential to usher in a new standard of care for men with prostate cancer requiring androgen deprivation therapy,” said Neal Shore, M.D., medical director of the Carolina Urologic Research Center and HERO program steering committee member. “For the first time, we now have a once-daily oral treatment that effectively and rapidly suppresses testosterone, with a safety analysis showing a lower incidence of major adverse cardiovascular events compared to leuprolide injections, the current standard of care, as evaluated in the Phase 3 HERO study. The COVID-19 pandemic has heightened the importance of oral treatments as men with prostate cancer continue to experience difficulties and risks traveling to receive injections.”
“Prostate cancer is a very personal journey, but a universal truth is that those of us living with this disease want better treatments and options. That is why the approval of Orgovyx is such an exciting milestone that brings a long-awaited oral treatment option to men with advanced prostate cancer,” said Thomas Farrington, president and founder of the Prostate Health Education Network. “It is so important for men to speak with their doctor and explore what treatment is right for them as they focus on their overall health.”
“With the approval of Orgovyx, men with advanced prostate cancer now have a new oral treatment option that has demonstrated robust efficacy and safety, all with one pill taken once-a-day,” said Lynn Seely, M.D., chief executive officer of Myovant Sciences, Inc. “We have successfully built our commercial capabilities to bring this newly approved treatment to the urologists and oncologists who care for men with advanced prostate cancer, with the goal of establishing Orgovyx as the new standard of care. We are incredibly grateful to the men and investigators who participated in the HERO study and to the FDA for expediting the review and approval of Orgovyx through its Priority Review pathway.”
In the Phase 3 HERO study, Orgovyx met the primary endpoint and achieved sustained testosterone suppression to castrate levels (< 50 ng/dL) through 48 weeks in 96.7% (95% confidence interval [CI]: 94.9-97.9) of men, compared with 88.8% (95% CI: 84.6-91.8) of men receiving leuprolide acetate injections, the current standard of care. Orgovyx also achieved several key secondary endpoints compared to leuprolide acetate, including suppression of testosterone to castrate levels at Day 4 and Day 15 (56% versus 0% and 99% versus 12%, respectively) and profound suppression of testosterone (< 20 ng/dL) at Day 15 (78% versus 1%). Orgovyx lowered prostate-specific antigen (PSA), on average, by 65% at Day 15 and by 83% at Day 29. In a substudy, 55% of men treated with Orgovyx achieved normal testosterone levels (> 280 ng/dL) or returned to baseline within 90 days of treatment discontinuation. The most frequent adverse events reported in at least 10% of men in the Orgovyx group were hot flush, musculoskeletal pain, fatigue, constipation, and mild to moderate diarrhea. The HERO data were previously presented in an oral presentation at the 2020 American Society of Clinical Oncology (ASCO) Virtual Scientific Program, with simultaneous publication in the New England Journal of Medicine.
https://en.wikipedia.org/wiki/Relugolix
FDA Approves Orgovyx (relugolix) as the First Oral Gonadotropin-Releasing Hormone (GnRH) Receptor Antagonist for Advanced Prostate Cancer
Monday, February 8, 2021
FDA Approves Gemtesa (vibegron) Tablets for the Treatment of Patients with Overactive Bladder (OAB)
Urovant Sciences (Nasdaq: UROV) announced the U.S. Food and Drug Administration (FDA) approval of the New Drug Application (NDA) for once-daily 75 mg Gemtesa (vibegron), a beta-3 adrenergic receptor (β3) agonist, for the treatment of overactive bladder (OAB) with symptoms of urge urinary incontinence (UUI), urgency, and urinary frequency in adults. This approval marks the first new oral branded OAB medication approved by the FDA since 2012, and it is the first product approval for Urovant Sciences.
“The FDA’s approval of Gemtesa is an important milestone for the tens of millions of patients living with overactive bladder and for Urovant, as it is our first drug approval. We look forward to launching Gemtesa in the coming months and believe that it will provide a compelling alternative for the many patients suffering from the burden of an overactive bladder. We also remain committed to bringing more new therapies to market that address unmet medical needs of patients suffering from urologic diseases,” said Jim Robinson, president and chief executive officer of Urovant Sciences.
“The clinical data for once-daily 75 mg Gemtesa demonstrated clear efficacy on the key symptoms of OAB by reducing urinary frequency, urge urinary incontinence, and urgency. In addition, data specifically showing reduction in urgency episodes are included in the Prescribing Information of Gemtesa, which is unique among currently-available OAB treatments. Urgency episode reduction data are particularly relevant for OAB patients and their health care providers, as they show Gemtesa’s direct impact on a hallmark symptom of the condition,” said Cornelia Haag-Molkenteller, M.D., Ph.D., chief medical officer of Urovant Sciences. “By successfully treating clinical symptoms, Gemtesa may allow patients to overcome the devastating impact that OAB can have on their daily lives.”
Gemtesa is an oral, once-daily tablet containing 75 mg of vibegron, a small-molecule β3 agonist which helps relax the detrusor bladder muscle so that the bladder can hold more urine, thereby reducing symptoms of OAB.
“Gemtesa is the first beta 3-agonist available as a once-daily pill which does not require dose titration,” said David Staskin, MD, clinical trial investigator and a leading urologist with St. Elizabeth’s Medical Center in Boston. “Notably, Gemtesa did not have any increase in the adverse event of hypertension compared to placebo in the key EMPOWUR study and has no interactions with medications metabolized by CYP2D6, which is important since many common medications are metabolized by CYP2D6.”
The FDA’s approval is based on results from an extensive development program involving more than 4,000 OAB patients, including the 12-week double blind, placebo-controlled Phase 3 EMPOWUR study with a dose of 75 mg and the double blind EMPOWUR long term extension study.1 These data show that treatment with Gemtesa resulted in statistically significant reductions in daily UUI, micturitions, and urgency episodes and an increase in the volume voided when compared to placebo in EMPOWUR.
The most common adverse reactions of Gemtesa from the double blind, placebo-controlled EMPOWUR study in ≥2% of patients were headache, nasopharyngitis, diarrhea, nausea, and upper respiratory tract infection. Gemtesa demonstrated the same rates for the adverse events of hypertension and increased blood pressure as placebo.
Saturday, February 6, 2021
FDA Approves Orladeyo (berotralstat) as the First Oral, Once-Daily Therapy to Prevent Attacks in Hereditary Angioedema Patients
BioCryst Pharmaceuticals, Inc. (Nasdaq: BCRX) announced the U.S. Food and Drug Administration (FDA) approval of oral, once-daily Orladeyo (berotralstat) for prophylaxis to prevent attacks of hereditary angioedema (HAE) in adults and pediatric patients 12 years and older.
“Orladeyo offers people with HAE and their physicians the first orally administered non-steroidal option for preventing HAE attacks and represents an important and welcome step in making more treatment options available to physicians and patients,” said Anthony J. Castaldo, president and chief executive officer of the US Hereditary Angioedema Association (HAEA).
In the pivotal Phase 3 APeX-2 trial, Orladeyo significantly reduced attacks at 24 weeks, and this reduction was sustained through 48 weeks. HAE patients who completed 48 weeks of treatment (150 mg) saw reductions in their HAE attack rates, from a mean of 2.9 attacks per month at baseline to a mean of 1.0 attacks per month after 48 weeks of therapy. In the long-term open label APeX-S trial, patients completing 48 weeks of therapy (150 mg) had a mean attack rate of 0.8 attacks per month.
Orladeyo was safe and well tolerated in both trials. The most frequently reported adverse reactions in patients receiving Orladeyo compared with placebo were gastrointestinal reactions. These reactions generally occurred early after initiation of treatment with Orladeyo, became less frequent with time and typically self-resolved.
“Patients and physicians acknowledge that HAE treatments can add a burden to patients’ lives. As an oral, once-daily option, Orladeyo can provide significant attack reduction and lessen the burden associated with injections and infusions,” said Marc Riedl, M.D., professor of medicine and clinical director, U.S. Hereditary Angioedema Association Center at the University of California, San Diego, and an investigator in the APeX-2 trial.
“With this new treatment option, physicians and patients can continue to have collaborative discussions to choose the treatment that meets each patient’s needs, life circumstances and preferences,” Riedl added.
HAE patients note a significant treatment burden associated with existing prophylactic therapy. In addition to reducing HAE attack rate, data from APeX-2 show that patients reported meaningful improvements in both quality of life and overall patient-reported satisfaction, and significant reductions in their monthly use of standard of care on-demand medicine, while taking oral, once-daily Orladeyo (150 mg).2,3
“The FDA approval of Orladeyo fulfills a promise BioCryst made to HAE patients that we were committed to helping them achieve the dream of an oral, once-daily medicine to prevent and reduce the burden of their attacks,” said Jon Stonehouse, president and chief executive officer of BioCryst.
“Thank you to the HAE patients who participated in our clinical trials, to the investigators around the world who conducted these trials, to the HAEA for their patient advocacy and to our employees who never forgot that patients were waiting. We will stay focused on enabling access and providing personalized support to HAE patients and physicians,” Stonehouse added.








