In continuation of my update on empagliflozin/linagliptin/metformin


The U.S. Food and Drug Administration (FDA) has approved Trijardy XR (empagliflozin/linagliptin/metformin hydrochloride extended release tablets) to lower blood sugar in adults with type 2 diabetes, along with diet and exercise. Trijardy XR provides three type 2 diabetes medicines in one pill, including Jardiance® (empagliflozin), Tradjenta® (linagliptin) and metformin hydrochloride extended release. Trijardy XR is marketed by Boehringer Ingelheim Pharmaceuticals, Inc. and Eli Lilly and Company (NYSE: LLY).
"Many adults living with type 2 diabetes who are already on a treatment plan including multiple medications still struggle to keep their blood sugar under control, and may require additional agents to reach their A1C targets," said Ralph DeFronzo, M.D., professor and diabetes division chief, UT Health San Antonio. "Adding new medicines to an individual's plan can be challenging for some, which is why new treatment options that can help improve blood sugar without the burden of an increased pill count are important. In addition, type 2 diabetes is a complex disease that often requires the use of multiple antidiabetic medications to improve glycemic control. Having three different diabetes medications in a single tablet is an important advance in diabetes treatment."
In the U.S., both Jardiance and Tradjenta are once-daily tablets used along with diet and exercise to lower blood sugar in adults with type 2 diabetes. Jardiance is also approved to reduce the risk of cardiovascular death in adults with type 2 diabetes who have known cardiovascular disease. Jardiance is not for people with type 1 diabetes or for people with diabetic ketoacidosis (increased ketones in the blood or urine). Tradjenta is not for people with type 1 diabetes or for the treatment of diabetic ketoacidosis. Tradjenta has not been studied in people with a history of pancreatitis and it is unknown if using Tradjenta increases the risk of developing pancreatitis in these people.
"We are proud to offer Trijardy XR as a new once-daily option combining three well-established medicines, including an extended-release version of metformin, the most commonly prescribed initial treatment for type 2 diabetes, Jardiance, the most prescribed SGLT2 inhibitor, and Tradjenta, the only single-dose DPP-4 inhibitor," said Mohamed Eid, M.D., M.P.H., M.H.A., vice president, Clinical Development & Medical Affairs, Cardio-Metabolism & Respiratory Medicine, Boehringer Ingelheim Pharmaceuticals, Inc. "We believe Trijardy XR has the potential to help adults with type 2 diabetes conveniently manage their treatment, especially those who are taking other medications and working on the necessary lifestyle changes."
Trijardy XR is not recommended for people with type 1 diabetes or diabetic ketoacidosis (increased ketones in the blood or urine). Trijardy XR has not been studied in patients with a history of pancreatitis. It is unknown whether patients with a history of pancreatitis are at an increased risk for the development of pancreatitis while using Trijardy XR. The labeling for Trijardy XR contains a warning for lactic acidosis, a rare but serious complication that can occur due to metformin accumulation, and is common to all products containing metformin.
The FDA approval of Trijardy XR is based on two randomized open-label trials that assessed the bioequivalence of empagliflozin, linagliptin and metformin hydrochloride extended release fixed-dose combination tablets and their individual components in healthy adults. The safety profile of Trijardy XR was found to be consistent with its individual components.
"The approval of Trijardy XR reflects our commitment to the diabetes community and to innovation that addresses evolving needs," said Jeff Emmick, M.D. Ph.D., vice president, Product Development, Lilly. "We developed Trijardy XR because many people with type 2 diabetes need help managing this complex condition without adding more pills to their treatment plan. We look forward to making this new option available soon."
Trijardy XR is not for people who have severe kidney problems, end stage renal disease, or are on dialysis, have a serious condition called metabolic acidosis or diabetic ketoacidosis (increased ketones in the blood or urine), or are allergic to Jardiance, Tradjenta, metformin, or any of the ingredients in Trijardy XR. There have been postmarketing reports of acute pancreatitis, including fatal pancreatitis, in patients taking linagliptin, a component of Trijardy XR. Take careful notice of potential signs and symptoms of pancreatitis. If pancreatitis is suspected, promptly discontinue Trijardy XR and initiate appropriate management. It is unknown whether patients with a history of pancreatitis are at increased risk for the development of pancreatitis while using Trijardy XR.
Trijardy XR will be available in four different dosages, including: 5 mg empagliflozin/2.5 mg linagliptin/1000 mg metformin HCl extended-release; 10 mg empagliflozin/5 mg linagliptin/1000 mg metformin HCl extended-release; 12.5 mg empagliflozin/2.5 mg linagliptin/1000 mg metformin HCl extended-release; and 25 mg empagliflozin/5 mg linagliptin/1000 mg metformin HCl extended-release.
What is Trijardy XR?
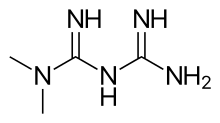
Trijardy XR is a prescription medicine that contains 3 diabetes medicines, empagliflozin (JARDIANCE), linagliptin (TRADJENTA), and metformin hydrochloride. Trijardy XR can be used along with diet and exercise to lower blood sugar in adults with type 2 diabetes, and in adults with type 2 diabetes who have known cardiovascular disease when empagliflozin (JARDIANCE), one of the medicines in Trijardy XR, is needed to reduce the risk of cardiovascular death.
Trijardy XR is not for people with type 1 diabetes, or for people with diabetic ketoacidosis (increased ketones in the blood or urine).
If you have had pancreatitis (inflammation of the pancreas) in the past, it is not known if you have a higher chance of getting pancreatitis while you take Trijardy XR.
https://www.drugs.com/history/trijardy-xr.html






