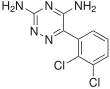
AbbVie (NYSE: ABBV), a research-based global biopharmaceutical company, today announced that the U.S. Food and Drug Administration (FDA) has approved Rinvoq (upadacitinib), a 15 mg, once-daily oral Janus kinase (JAK) inhibitor, for the treatment of adults with moderately to severely active rheumatoid arthritis (RA) who have had an inadequate response or intolerance to methotrexate (MTX-IR).1 Rinvoq is expected to be available in the U.S. in late August 2019.
The FDA approval of Rinvoq is supported by data from the SELECT program, one of the largest registrational Phase 3 programs in RA with approximately 4,400 patients evaluated across all treatment arms in five studies.2-6 The studies include assessments of efficacy, safety and tolerability across a variety of RA patients, including those who failed or were intolerant to biologic disease-modifying anti-rheumatic drugs and who were naïve or inadequate responders to methotrexate. Rinvoq is not indicated for methotrexate-naïve patients.
"Despite the availability of multiple treatment options with varying mechanisms of action, many patients still do not achieve clinical remission or low disease activity—the primary treatment goals for rheumatoid arthritis," said Roy M. Fleischmann, M.D., primary investigator for SELECT-COMPARE and clinical professor at the University of Texas Southwestern Medical Center at Dallas. "With this FDA approval, Rinvoq has the potential to help additional people living with RA achieve remission who have not yet reached this goal."
Across the SELECT Phase 3 studies, Rinvoq met all primary and ranked secondary endpoints. The primary endpoints include:
- In SELECT-EARLY, 52 percent of MTX-naïve patients treated with Rinvoq 15 mg achieved ACR50 vs 28 percent treated with MTX at week 121
- In SELECT-MONOTHERAPY, 68 percent of MTX-IR patients treated with Rinvoq 15 mg achieved ACR20 vs 41 percent treated with continued MTX at week 141
- In SELECT-COMPARE, 71 percent of MTX-IR patients treated with Rinvoq 15 mg plus MTX achieved ACR20 vs 36 percent treated with placebo plus MTX at week 121
- In SELECT-NEXT, 64 percent of csDMARD-IR patients treated with Rinvoq 15 mg plus csDMARDs achieved ACR20 vs 36 percent treated with placebo plus csDMARDs at week 121
- In SELECT-BEYOND, 65 percent of biologic-IR patients treated with Rinvoq 15 mg plus csDMARDs achieved ACR20 vs 28 percent treated with placebo plus csDMARDs at week 121
"The discovery and development of Rinvoq is indicative of AbbVie's long-standing commitment to advancing the science for people living with immune-mediated conditions," said Michael Severino, M.D., vice chairman and president, AbbVie. "Today's FDA approval marks an important milestone in our pursuit to deliver innovative medicines that advance care for people living with rheumatoid arthritis."
Clinical Remission
Patients taking Rinvoq achieved clinical remission, a state characterized by almost no disease activity and symptoms, even without methotrexate.2-3,6 Approximately 30 percent of patients treated with Rinvoq achieved clinical remission (as assessed by DAS28-CRP<2.6) at week 12 in SELECT-COMPARE and week 14 in SELECT-MONOTHERAPY compared to six percent with placebo plus methotrexate and eight percent with methotrexate, respectively.1 In SELECT-EARLY, 36 percent of patients treated with Rinvoq achieved clinical remission (as assessed by DAS28-CRP<2.6) at week 12 compared to 14 percent with methotrexate.1
Durable remission rates were observed up to week 26. Forty-eight percent of patients treated with Rinvoq alone in SELECT-EARLY and 41 percent of patients treated with Rinvoq plus methotrexate in SELECT-COMPARE achieved clinical remission at weeks 24 and 26, compared to nine percent with placebo plus methotrexate and 18 percent with methotrexate, respectively.1 Analysis at weeks 24 and 26 were not controlled for multiple comparisons.3,10
Radiographic Inhibition
Rinvoq significantly inhibited radiographic progression as measured by the change in modified total Sharp score (mTSS) from baseline compared to methotrexate in SELECT-EARLY (0.14 vs 0.67) and Rinvoq plus methotrexate compared to placebo plus methotrexate in SELECT-COMPARE (0.15 vs 0.78) through weeks 24 and 26, respectively.1
Safety
The most common side effects associated with Rinvoq include upper respiratory tract infections (common cold, sinus infections), nausea, cough and pyrexia.1 Patients treated with Rinvoq are at increased risk for developing serious infections that may lead to hospitalization or death. These infections include tuberculosis (TB), invasive fungal, bacterial, viral, and other infections due to opportunistic pathogens. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.1 Lymphoma and other malignancies have been observed in Rinvoq-treated patients.1 Thrombosis, including deep vein thrombosis, pulmonary embolism, and arterial thrombosis, have occurred in patients treated with JAK inhibitors used to treat inflammatory conditions.1 Patients treated with RINVOQ also may be at risk for other serious adverse reactions, including gastrointestinal perforations, neutropenia, lymphopenia, anemia, lipid elevations, liver enzyme elevations, and embryo-fetal toxicity.1
Ease of Use and Access
Designed to help accommodate the physical limitations of people living with RA, the packaging for Rinvoq includes a bottle cap with a wide, easy-to-grip texture and an embedded tool that punctures the foil liner to simplify medication access. This packaging design was awarded the Arthritis Foundation Ease of Use Commendation.
"Rheumatoid arthritis can have a debilitating impact on the lives of those with the chronic disease, including making it difficult to perform everyday tasks," said Cindy McDaniel, senior vice president, consumer health, Arthritis Foundation. "The Arthritis Foundation is committed to recognizing innovation that can help patients living with rheumatoid arthritis and we are proud to recognize AbbVie with our Ease of Use Commendation for the packaging design of Rinvoq."
AbbVie continues to work closely with key stakeholders to support patient access to Rinvoq, including offering a patient support program and a co-pay card that may reduce out-of-pocket costs to $5 per month for eligible, commercially-insured patients. For those with limited or no health insurance, AbbVie offers myAbbVie Assist, a patient assistance program that provides Rinvoq to qualifying patients.
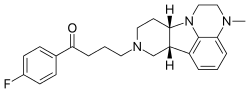
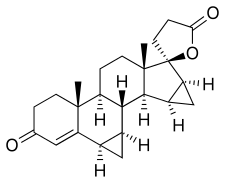
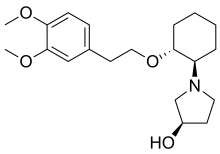
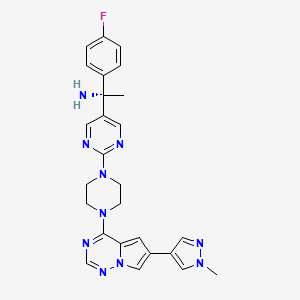
https://en.wikipedia.org/wiki/Upadacitinib
https://www.drugbank.ca/drugs/DB15091