In continuation of my update on Venclexta (venetoclax)

AbbVie a research-based global biopharmaceutical company, announced that the U.S. Food and Drug Administration (FDA) has approved Venclexta (venetoclax) in combination with obinutuzumab (Gazyva®) for previously untreated patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). The FDA granted Breakthrough Therapy designation for this combination therapy, and early submission of the data was provided under the Real-Time Oncology Review (RTOR) pilot program, which led to approval in just over two months, following submission of the complete application.
"This FDA approval provides a new chemotherapy-free combination treatment option for patients, and underscores the growing utility of Venclexta in CLL," said Michael Severino, M.D., vice chairman and president, AbbVie. "The approval is based on findings from the CLL14 trial in which patients received a 12-month treatment regimen. The majority of patients receiving Venclexta in the trial remained progression-free at two years."
Data from the CLL14 trial is expected to be presented at an upcoming medical meeting and published in a journal this year.
"Patients never treated for their CLL have had to rely largely on chemotherapy as their initial treatment," said Michael Hallek, M.D., lead investigator of the CLL14 study, Department of Internal Medicine and Center of Integrated Oncology at the University Hospital Cologne in Germany, and Head of the German CLL Study Group. "The approval of the Venclexta combination means that patients with previously untreated CLL now have a finite duration, chemotherapy-free treatment option that can allow them to live longer without disease progression, induce high rates of minimal residual disease (MRD) negativity and, importantly, allow them to complete their course of therapy within 12 months. This is a major step forward in how previously untreated CLL is managed and further supports the growing benefits offered by Venclexta in CLL."
The CLL14 trial demonstrated superior progression-free survival as assessed by an independent review committee (PFS; the time from initiation of treatment until disease progression or death) in patients treated with Venclexta plus obinutuzumab compared to patients who received chlorambucil plus obinutuzumab, a commonly used standard of care. With a median follow-up of 28 months (range: 0.1 to 36 months), Venclexta plus obinutuzumab reduced the risk of progression or death by 67% compared with chlorambucil plus obinutuzumab (hazard ratio: 0.33, 95% confidence interval [CI]: 0.22, 0.51; p<0.0001).1 Median PFS was not reached in either treatment arm.1 Minimal residual disease (MRD) negativity (undetectable disease in the blood or bone marrow) was assessed as a secondary endpoint and occurs when less than one CLL cell per 10,000 leukocytes can be detected using sensitive analytical methods. Higher rates of MRD negativity were observed with Venclexta plus obinutuzumab compared to obinutuzumab plus chlorambucil in both bone marrow (57% versus 17%, p<0.0001) and peripheral blood (76% versus 35%, p<0.0001) three months after treatment completion .
In the CLL14 trial, adverse events (AEs) were consistent with the known safety profiles of Venclexta and obinutuzumab alone. Serious adverse reactions (ARs) were reported in 49% of patients in the Venclexta plus obinutuzumab arm, most often due to febrile neutropenia and pneumonia (5% each). The most common ARs (≥15%) of any grade were neutropenia (60%), diarrhea (28%), fatigue (21%), nausea (19%), anemia (17%), and upper respiratory tract infection (17%).
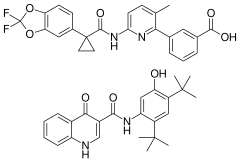
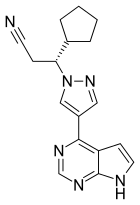
Venclexta, an oral B-cell lymphoma-2 (BCL-2) inhibitor, has been granted five Breakthrough Therapy designations from the FDA.
https://en.wikipedia.org/wiki/Venetoclax