In continuation of my update on benzodiazepine
In the first 90 days of concurrent opioid and benzodiazepine use, the risk of opioid-related overdose increases five-fold compared to opioid-only use among Medicare recipients, according to a new study from the University of Pittsburgh School of Pharmacy, published today in JAMA Network Open.
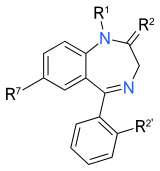
The U.S. Centers for Disease Control and Prevention recommends against concurrent use of opioids and benzodiazepines, but nearly a quarter of Medicare recipients who are prescribed opioids also fill prescriptions for benzodiazepines. Both drugs have sedative effects.
"Patients who must be prescribed both an opioid and a benzodiazepine should be closely monitored by health care professionals due to an increased risk for overdose, particularly in the early days of this medication regimen," said Inmaculada Hernandez, Pharm.D., Ph.D., assistant professor at Pitt's School of Pharmacy and the study's lead author. "Moving forward, policy interventions should focus on preventing concurrent exposure instead of simply reducing the length of time patients use both drugs."
Hernandez and her team used 2013-2014 Medicare Part D data to assess how the duration of simultaneous exposure to the two types of drugs impacts the risk of overdose. Beneficiaries not being treated for cancer who filled at least one opioid prescription during that year were included in the analysis, which ultimately looked at more than 71,000 beneficiaries who averaged 66.5 years of age.
Patients were divided into two groups, those with a supply of only opioids the day before an overdose, and those with an opioid and benzodiazepine supply. The second group was then divided into four subgroups based on the cumulative number of days with overlapping opioid and benzodiazepine supplies.
For patients who did not have an overdose event in the first 90 days of concurrent use, overdose risk in the next 90 days decreased from five-fold to less than double, which is still elevated compared to opioid-only use. After 180 days of concurrent use, the risk of overdose was no higher than the risk for opioid-only use.
Results were adjusted to account for patient demographics, health insurance factors, clinical characteristics, and the number of unique clinicians who prescribed opioids or benzodiazepines to the patients.
Hernandez and her team also found that a beneficiary's risk of concurrent opioid and benzodiazepine use and of overdose increased with the numbers of opioid and benzodiazepine prescribers. In other words, the more clinicians prescribing medications to a beneficiary, the higher the risk of that beneficiary overdosing.
"These findings demonstrate that fragmented care plays a role in the inappropriate use of opioids, and having multiple prescribers who are not in communication increases the risk for overdose," said Yuting Zhang, Ph.D., director, Pharmaceutical Economics Research Group, Health Policy and Management, Pitt Graduate School of Public Health, and the study's senior author. "Prescription monitoring programs and policy interventions can help curb this problem and reduce risk for patients."