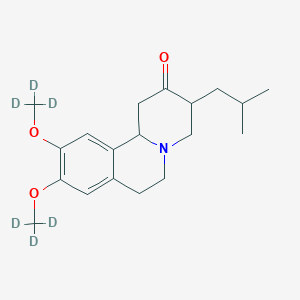
Ezetimibe atorvastatin
In the first major trial of its kind, Cleveland Clinic researchers used a blinded rechallenge with atorvastatin or placebo to objectively confirm the presence of muscle-related symptoms in patients with a history of intolerance to multiple statins and found that evolocumab (a PCSK9 inhibitor) was a more effective option to lower cholesterol than ezetimibe in these patients.
The double-blinded, placebo-controlled clinical trial was designed with two stages:
- In Phase A, patients were assigned to two groups. Each group was treated for 10 weeks with atorvastatin or placebo in a blinded fashion, then crossed over to the alternate therapy for another 10 weeks. Patients were asked to report any muscle pain or weakness.
- Patients who reported intolerable muscle symptoms on atorvastatin, but not placebo, moved to Phase B. In this 24-week phase, patients with confirmed statin intolerance were administered two alternative non-statin therapies, ezetimibe vs. evolocumab.
- The research is being presented at the American College of Cardiology's 65th Annual Scientific Session and simultaneously published online in the Journal of the American Medical Association."Statin intolerance has been a very challenging clinical problem," said Steven Nissen, M.D., chairman of Cardiovascular Medicine at Cleveland Clinic. "The study showed that PCSK9 inhibitors can significantly lower cholesterol in patients with documented statin intolerance, providing an effective treatment for these difficult to manage patients."The GAUSS-3 trial enrolled 511 patients with very high levels of LDL cholesterol - averaging more than 210 mg/dL ¬¬- and with a history of muscle-related statin intolerance. More than 80% of participants had previously reported intolerance to three or more statins. The study showed that 42.6 percent of these patients reported muscle pain or weakness on atorvastatin, but not placebo, and 26.5 percent on the placebo, but not atorvastatin.