Third-generation tyrosine kinase inhibitor (TKI) study findings suggest that bosutinib is associated with a low risk of vascular and cardiac events in patients undergoing first-line or subsequent treatment for chronic myeloid leukaemia (CML).
"The results of this analysis suggest that the vascular and cardiac toxicity profile of bosutinib is distinct relative to other TKIs", write Jorge Cortes, from University of Texas MD Anderson Cancer Center in Houston, USA, and co-authors in the American Journal of Hematology
.
The team collated information on treatment-emergent adverse events (TEAEs) in 570 patients who received second-, third- or fourth-line bosutinib treatment for Philadelphia chromosome-positive CML as part of a phase I/II study.
In addition, the researchers determined the incidence of TEAEs in a phase III study comparing first-line bosutinib in 248 patients with first-line imatinib in 251 patients.
Trial participants were all followed up for at least 2 years and the overall incidence of vascular TEAEs was low, with all-grade and grade 3 or more severe side effects affecting 6.8% and 3.7% of patients given bosutinib, respectively.
First-line bosutinib was associated with a lower rate of vascular TEAEs than second-line or subsequent bosutinib therapy, affecting 4.8% versus 7.7%. First-line imatinib had comparable incidence of both overall and grade 3 and more severe vascular TEAEs to that of first-line bosutinib.
Cerebrovascular TEAEs were reported in 1.8% of patients given bosutinib, again being less common in those given primary bosutinib relative to second-line or later treatment (0.8 vs 2.3%). All-grade and grade 3 or more severe cardiovascular TEAEs occurred in 3.7% and 2.3% of bosutinib-treated patients, occurring at a lower rate in first-line than later treated patients (2.4 vs 4.2%).
Serious vascular TEAEs were reported in 4.2% of bosutinib-treated patients, with grade 3 or more severe events occurring in 3.1%, most commonly coronary artery disease (0.9%) and acute myocardial infarction (0.6%).
Events were less common in newly diagnosed patients than those with refractory or relapsed disease (2.0 vs 5.1%), and there was no significant difference in the incidence or exposure-adjusted rate between the first-line bosutinib and imatinib groups.
Ref : http://onlinelibrary.wiley.com/doi/10.1002/ajh.24360/abstract
Bosutinib shows 'low' vascular, cardiac event risk profile: Third-generation tyrosine kinase inhibitor study findings suggest that bosutinib is associated with a low risk of vascular and cardiac events in patients undergoing first-line or subsequent treatment for chronic myeloid leukaemia.








 (Ambrisentan)
(Ambrisentan) 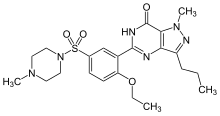 (Sildenafil)
(Sildenafil) In continuation of my update on
In continuation of my update on