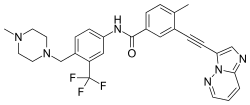
In continuation of my update on Ponatinib
Ponatinib is highly active when given to patients within 6 months of developing chronic phase chronic myeloid leukaemia (CML), phase II results show, but its toxicity profile is unacceptable for first-line treatment.
The investigators, from the University of Texas MD Anderson Cancer Center in Houston, USA, report “deep and early responses” to the third-generation tyrosine kinase inhibitor (TKI) in The Lancet Haematology.
“However, due to the risk of vascular thrombotic events and the availability of alternative options for these patients, other drugs should be considered first in the frontline setting”, recommend Jorge Cortes and co-authors.
At 6 months, a complete cytogenetic response (CCyR) was achieved by 94% of 46 assessed patients and a major molecular response (MMR, BCR–ABL1 ≤0.1%) by 83%, with undetectable levels of BCR–ABL1 in 22% of assessed patients and a level of 1% or below in 96%.
The median times to a complete haematological response, CCyR and MMR were 0.6, 2.89 and 2.90 months, respectively, and there was 100% overall and transformation-free survival after 2 years.
But the initial starting dose of 45 mg/day in 43 patients was reduced to 30 mg/day or 15 mg/day for 18 patients after tolerability issues, while six of eight patients started on 30 mg/day had the dose reduced to 15 mg/day. At least one treatment interruption was required by 85% of patients, while 88% had their dose reduced due to adverse events (66%) or US Food and Drug Administration (FDA) advice (24%).
All of these patients finally discontinued ponatinib therapy and switched to an alternative TKI following adverse events or FDA concerns about an increased risk of thromboembolism.
In all, 49% of patients experienced cardiac or vascular events and 22% had more than one such episode. These included worsening or new-onset of hypertension, one case each of acute coronary syndrome and myocardial infarction, and three cases of vaso-occlusive disease. Two patients experienced cerebrovascular events, and one patient developed pulmonary hypertension within a month of discontinuing ponatinib.
