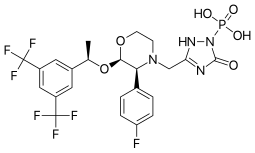
In continuation of my update on Selinexor

Patients with a form of blood cancer known as multiple myeloma who haven't responded to other therapies might have a new weapon against the disease, researchers say.
A drug called selinexor appeared to help patients with the blood and bone marrow cancer, according to a clinical trial involving 122 people.
"This study proved that a novel, first-in-class drug with a new mechanism of action can kill a patient's cancer cells," said study senior author Dr. Sundar Jagannath. He directs the multiple myeloma program at the Tisch Cancer Institute at Mount Sinai in New York City.
Selinexor also "worked in patients who had exhausted every other treatment and who would have been placed on hospice care otherwise," Jagannath said in a hospital news release.
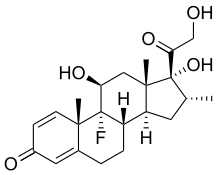
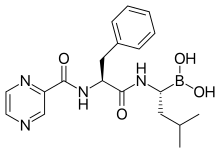
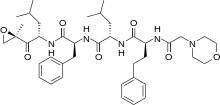
In the trial, which was funded by the drug's maker, Karyopharm, patients at centers in the United States and Europe received a combination therapy of two pills, selinexor and the standard anti-cancer medicine dexamethasone.
As reported in the Aug. 22 issue of the New England Journal of Medicine, nearly 40% of the patients showed at least a minimal response to the therapy within one or two months. There were "significant" responses in more than a quarter of the patients, the researchers said, and two patients had their cancers go into complete remission.
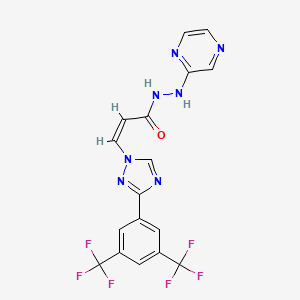
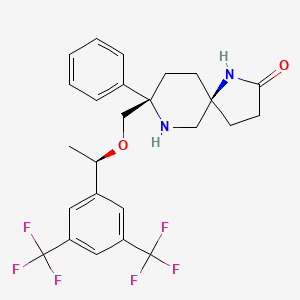
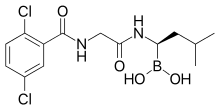
As the team explained, selinexor works in a new way to fight myeloma, blocking a key mechanism in cancer cell growth and causing the cell to die.
Although the drug caused no toxicity to organs, there were side effects for some patients. These included low blood counts without bleeding, nausea, vomiting, lack of appetite or fatigue.
The U.S. Food and Drug Administration had already approved selinexor in early July to treat patients with multiple myeloma resistant to multiple therapies.
"This study is meaningful for patients with multiple myeloma who haven't had success on multiple other therapies," said study first author Dr. Ajai Chari, director of clinical research in the multiple myeloma program at the Tisch Cancer Institute.
"An increasing number of patients have resistance to the standard drugs used in the treatment of multiple myeloma, and the overall survival in these patients is short, sometimes less than three months," Chari said in the news release.
One myeloma expert unconnected to the research was heartened by the findings.
The trial results are "cautiously positive and very encouraging," said hematologist Dr. Kanti Rai. He works in the CLL Research and Treatment Program at Northwell Health Cancer Institute in New Hyde Park, N.Y.
Rai noted that while newer drugs are helping many multiple myeloma patients, others are still left without viable treatment options.
"The need for better treatments is especially urgent for those patients who are elderly, have compromised functions of other vital organs, have had multiple chemotherapy regimens in the past and still have evidence of progressive disease," he explained. "For such patients, unfortunately, death seems imminent."
Rai called the advent of selinexor "a positive step forward for patients with myeloma who otherwise have no hope for the future."
For their part, the Tisch researchers said they are also assessing selinexor for treatment of multiple myeloma in combination with other approved multiple myeloma drugs, as well for treatment of other cancers such lymphoma and ovarian cancer.
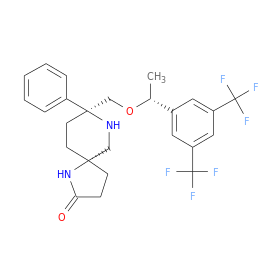
https://en.wikipedia.org/wiki/Selinexor