A drug that stimulates neuron pruning can nudge mice away from habit-driven behaviors when combined with retraining, neuroscientists have found.
The results were published online on November 30 by Nature Communications.


The drug fasudil, approved in Japan for cerebral vasospasm and stroke, inhibits an enzyme that stabilizes cells' internal skeletons. The researchers suggest that fasudil or similar compounds could be effective tools for facilitating the treatment of drug abuse and preventing relapse.
A large fraction of the actions people perform each day come from habits, not from deliberate decision making. Going on auto-pilot can free up attention for new things, but it can also be detrimental, in the case of drug abuse and drug-seeking behavior, says lead author Shannon Gourley, PhD, assistant professor of pediatrics, psychiatry and behavioral sciences at Emory University School of Medicine and Yerkes National Primate Research Center.
"Some habits are adaptive - for example, turning off a light when you exit a room - but others can be maladaptive, for example in the case of habitual drug use. We wanted to try to figure out a way to help 'break' habits, particularly those related to the highly-addictive drug cocaine," says Gourley.
Gourley and former graduate students Andrew Swanson, PhD and Lauren Depoy, PhD tested fasudil in situations where they had trained mice to poke their noses in two chambers, based on rewards of both food and cocaine. Then the researchers changed the rules of the game. The mice had to learn something new, in terms of where to poke their noses to get the reward.
In particular, the mice could now only get a reward from one chamber instead of both. Fasudil helped the mice adjust and display "goal-directed" behavior, rather than their previous habit-based behavior.
In addition, the researchers trained the mice to supply themselves a sweet cocaine solution. Then they changed the nature of that experience: the cocaine was paired with lithium chloride, which made the mice feel sick. Fasudil treatment nudged the mice to give themselves less cocaine afterwards, rather than continuing to respond habitually. The scientists envision this as modeling negative experiences associated with cocaine use in humans.
"Humans may seek treatment due to the negative consequences of cocaine abuse, but many people still relapse. We're trying to strengthen the goal of abstaining from drug taking," says Gourley.
The researchers conducted additional experiments that revealed that fasudil didn't make cocaine itself less pleasurable, but was specifically modifying the habit process. Also, fasudil did not affect other forms of decision making.
Un-learning of habits involves remodeling connections made by cells in the brain. In the mouse retraining experiments, the way that fasudil seems to work is that it promotes the pruning of dendritic spines. Dendritic spines are structures that help neurons communicate and embody the strength of connections between them.
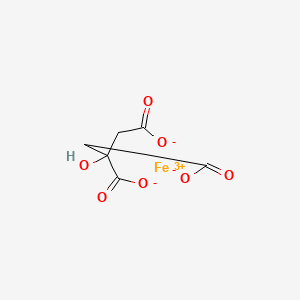
Fasudil inhibits Rho kinase, which stabilizes F-actin, a major component of cells' internal skeletons. Thus, it loosens up cell structures. And in mice, fasudil appears to slightly reduce the density of dendritic spines in a region of the brain that is important for learning new behaviors.
"In this context, we imagine that fasudil is optimizing signal-to-noise, so to speak, allowing this brain region to efficiently guide decision making," says Gourley.
When fasudil is given to the mice a day after training, no changes in spine density are seen, indicating that it must be paired with new learning to have that effect.
Some caution is order, because overactive synaptic pruning is proposed to play roles in Alzheimer's disease and schizophrenia. In their paper, the authors conclude:
Pairing Rho kinase inhibitors with cognitive behavioral therapy in humans could be an effective pharmacological adjunct to reduce the rate of relapse... Given its favorable safety profile and our evidence that it can mitigate cocaine self-administration, fasudil is a strong candidate, with the caveats that we envision it administered as an adjunct to behavioral therapy and potentially during early phases of drug withdrawal.
------







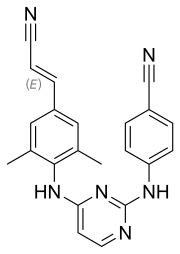 rilpivirine
rilpivirine  Dolutegravir
Dolutegravir