In continuation of my update on Tivozanib
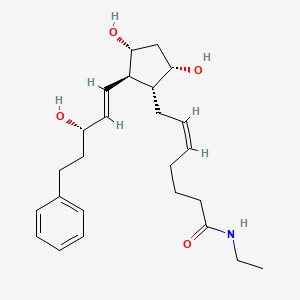
AVEO Oncology (Nasdaq: AVEO) announced the U.S. Food and Drug Administration (FDA) approval of Fotivda (tivozanib) for the treatment of adults with relapsed or refractory advanced renal cell carcinoma (RCC) who have received two or more prior systemic therapies. Fotivda is an oral, next-generation vascular endothelial growth factor (VEGF) tyrosine kinase inhibitor (TKI).
“Today’s approval of Fotivda provides a new tool for treating patients with kidney cancer who have relapsed or become refractory to two or more prior systemic therapies,” said Brian Rini, MD, Chief of Clinical Trials at Vanderbilt Ingram Cancer Center and principal investigator of the TIVO-3 trial. “With advances in RCC treatment, patients are living longer, increasing the need for proven, well tolerated treatment options in the relapsed or refractory setting. The TIVO-3 study is the first positive Phase 3 study in RCC patients who received two or more prior systemic therapies, and also the first Phase 3 RCC study to include a predefined population of patients who have received prior immunotherapy, the current standard of care in earlier-line treatment. With this approval, I believe Fotivda represents an attractive intervention, and expect it to play a meaningful role in the evolving RCC treatment landscape.”
“We believe in Fotivda’s potential to provide a differentiated treatment option for the growing number of individuals in the U.S. with relapsed or refractory RCC, and today marks the culmination of many years of hard work and determination of many individuals to bring this therapy to patients,” said Michael Bailey, president and chief executive officer of AVEO. “With today’s approval, AVEO begins its journey as a commercial-stage company, a noteworthy accomplishment in our industry. On behalf of the entire AVEO team, I would like to thank all the patients, their families, and caregivers whose tireless efforts made this day possible.”
“Relapsed or refractory RCC is a devastating disease for which patient outcomes can be limited due to the tradeoff between tolerability and efficacy,” said Dena Battle, president of KCCure. “The FDA approval of Fotivda represents an exciting, meaningful advancement by providing a new treatment option for this patient population.”
AVEO plans to make Fotivda available to patients in the U.S. by March 31, 2021.
The approval of Fotivda is based on AVEO’s pivotal Phase 3 study, TIVO-3, comparing Fotivda to sorafenib in relapsed or refractory advanced RCC following two or more prior systemic therapies. The application is also supported by three additional trials in RCC and includes safety data from over 1,000 clinical trial subjects.
Patients (n=350) enrolled in the TIVO-3 study were randomized 1:1 to receive either Fotivda or sorafenib. The main efficacy outcome measure was progression-free survival (PFS), assessed by a blinded independent radiology review committee. Other efficacy endpoints were overall survival (OS) and objective response rate (ORR).
Median PFS was 5.6 months (95% CI: 4.8, 7.3) in the Fotivda arm (n=175) compared with 3.9 months (95% CI: 3.7, 5.6) for those treated with sorafenib (HR 0.73; 95% CI: 0.56, 0.95; p=0.016). Median OS was 16.4 (95% CI: 13.4, 21.9) and 19.2 months (95% CI: 14.9, 24.2), for the Fotivda and sorafenib arms, respectively (HR 0.97; 95% CI: 0.75, 1.24). The ORR was 18% (95% CI: 12%, 24%) for the Fotivda arm and 8% (95% CI: 4%, 13%) for the sorafenib arm.
The most common (≥20%) adverse reactions were fatigue, hypertension, diarrhea, decreased appetite, nausea, dysphonia, hypothyroidism, cough, and stomatitis. The most common grade 3 or 4 laboratory abnormalities (≥5%) were decreased sodium, increased lipase, and decreased phosphate.
The recommended tivozanib dose is 1.34 mg once daily with or without food for 21 days every 28 days on treatment followed by 7 days off treatment (28 day cycle) until disease progression or unacceptable toxicity.
https://en.wikipedia.org/wiki/Tivozanib